![]()
![]()
(Topic Last Updated On: 06/05/2018)
The Billable Services menu item on the Accounting menu launches the Billable Services screen, which is used to configure each billable service rendered by your facility. The configured services determine how your patients will be charged for different types of rendered services depending on each patient's associated Payer/Rate Group and current, effective Billing Episode. This screen was enhanced significantly for Methasoft Version 6 to accommodate the comprehensive Accounting module functionality upgrade, implemented for third party medical billing and electronic billing claim export, while providing Self Pay-Only facilities with enhanced functionality. Six Billable Services are currently available for selection, and numerous Service Type and other configuration options are available for each. Optional fields are available for facilities using Methasoft to generate claims and/or export and submit claims to third party payers electronically. The 'Service Line Policy' field provides four options for configuring how service line data will be stored for generated claims. The 'Effective On' and 'Effective To' date fields allow users to schedule Rate changes in advance for a seamless transition to new rates per Payer/Rate Group. The Effective date range of a service can also be modified to dates in the past to accommodate unusual scenarios, allowing users to correct erroneous charge date by using the Charge Manager screen. The 2 screen shots below display common examples data details for configured Billable Services to charge for Dosing, along with other types of services on the grid:
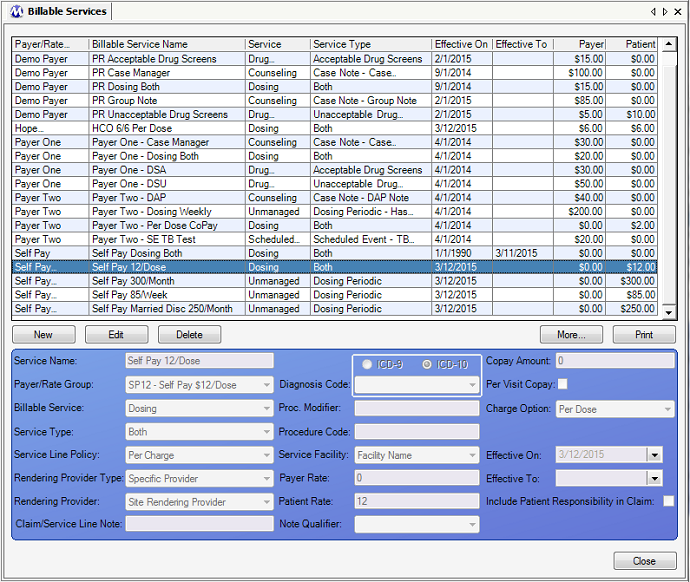
Billable Services - An Example Dosing - Both - Per Dose Service to Charge Self Pay Patients
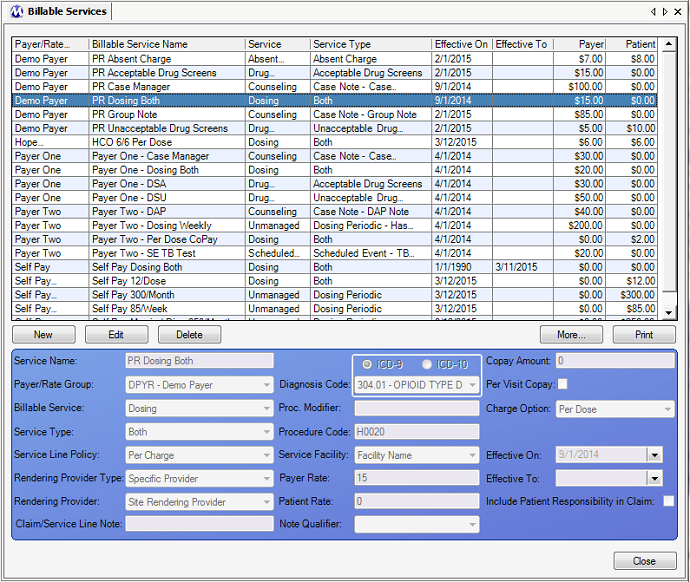
Billable Services - An Example Dosing - Both - Per Dose Service to Charge Third Party Payers via Exported Billing Claims
Service Name
This field is used for entering the name of the billable service being configured. Your facility should come up with the best possible naming convention after consideration of your facility's reporting needs for clarity. The name entered in this field is not exported to billing export files.
Payer/Rate Group
This field is used for selecting the payer/rate group which will be associated with the configured billable service. All patients associated with the selected payer/rate group, either via the Basic Dosing Charge Information screen, or via the Billing Episodes screen, will then be charged accordingly for the rendered service, provided that the effective date range of the service is current/effective, and that the date range of the patient's billing episode is current/effective. The list of available selections in this field is populated by all Payer/Rate Groups entered on the Payer/Rate Groups screen.
Billable Service
This field is used for selecting the billable service to configure (this can be thought of as the service 'category', 'primary type', or 'header type'). 6 options are available for selection in this field.
Absent Charge: This service is selected to set up a service to charge patients for failure to attend your facility as scheduled. Once this service is configured, patients with current/effective billing episodes associated with the selected payer/rate group will be charged the defined amount(s) if they are absent from their normal clinic attendance schedule. Such a patient's account(s) will be charged either when the nightly processes mark the patient as absent, or if an absent record is entered manually on the Absent Records screen.
Counseling: This service is selected to set up a service to charge patients for individual or group counseling sessions. Once this service is configured, patients with current/effective billing episodes associated with the selected payer/rate group will be charged the defined rate(s) when a case note of the specific 'Service Type' is entered in the system, based on the Note Date of the case note entered. The rate(s) charged are based on the number of 'Billable Units' entered with the case note record. If 1 billable unit is entered, then 1 x rate(s) will be charged. If 5 billable units are entered, then 5 x the rate(s) will be charged. See the 'Considerations' section below for more details on how to optimally configure your case note templates and counseling services.
Dosing: This service is selected to set up a service to charge for administering medication to patients. Once this service is configured, patients with current/effective billing episodes associated with the selected payer/rate group will be charged the defined rate(s) when a dosing transaction is recorded on the Dose Patient screen. The same or different rate(s) are charged Per Dose for window and/or takeout dose(s), depending on the 'Service Type' selected. (***Note: See 'Unmanaged' below - 'Unmanaged' billable services can be used to charge patients for dosing periodically in combination with a selected 'Service Type' and 'Charge Option', and potentially a 'Charge Day' depending on the other selections made.)
Drug Screens: This service is selected to set up a service to charge patients for drug screen tests. Once this service is configured, patients with current/effective billing episodes associated with the selected payer/rate group will be charged the defined rate(s) when a drug screen test result is either entered on the Drug Screen Results screen or is automatically downloaded via nightly processes. The 'Service Type' selected will determine whether or not patients are charged for 'Acceptable' (clean/passing) test results and/or for 'Unacceptable' (dirty/failing) test results entered. To charge for both Acceptable and Unacceptable results, 2 billable services must be entered, 1 for Acceptable, and another for Unacceptable.
Scheduled Events: This service is selected to set up a service to charge patients for scheduled events the patient is scheduled to attend. Once this service is configured, patients with current/effective billing episodes associated with the selected payer/rate group will be charged the defined rate(s) when a scheduled event they are scheduled to attend is Completed (or updated with a 'Complete' status) via various screens throughout Methasoft. See the 'Considerations' section below related to using Scheduled Event billable services vs. using Additional Charge functionality available on the Patient Payments screen to evaluate the advantages and disadvantages of using either.
Unmanaged: This service is selected to set up a Dosing service to charge patients periodically for dosing transactions, in lieu of charging patients at the time dosing transactions are entered on the Dose Patient screen. Once this service is configured, patients with current/effective billing episodes associated with the selected payer/rate group will be charged the defined rate(s) based on the 'Service Type' and/or 'Charge Option'/'Charge Day' selected. Charges are generated by nightly processes for Unmanaged billable services. The term 'Unmanaged' is used to describe this type/category of service because the charges are generated periodically by nightly processes, instead of being associated directly with another system transaction, such as the entry of a case note record or recording of a dosing transaction. ***Note: It is very important to understand that selecting a 'Charge Option' for an Unmanaged service only matters if 'Dosing Periodic' is selected as the 'Service Type' (see below), because the other 3 available 'Service Type' selections all trigger unique functionality that ignores 'Charge Option' settings. See the 'Considerations' section below regarding the use of Unmanaged billable services, service types and charge options.
Service Type
This field is used for selecting the specific type of the 'Billable Service' selected in the field above it. Available selections will vary in this field depending on which 'Billable Service' is selected. Below is an explanation of the options available for each 'Billable Service', which are represented in parentheses:
(Absent Charge) Absent Charge: This is the only available selection for the 'Absent Charge' billable service. The charge will be created either when the nightly processes mark a patient as absent, or if an absent record is entered on the Absent Records screen.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines is the 'Absent Date', which can be viewed for any absent record on the Absent Records screen. This date should be the date the patient was scheduled to attend the facility, based on attendance schedule data stored on the Dosing Information screen, and failed to attend. If an Absent record is deleted on the Absent Records screen, the associated charge will be deleted automatically.
(Counseling) Case Note - (Note Type): This service applies only to the selected case note type. Only case note types marked as 'Billable' on the Case Note Templates screen will be available for selection in this field. The charge will be created at the time the billable case note is saved on the Case Notes screen, and the rate(s) charged are based on the number of Billable Units entered for the case note.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines is the 'Note Date', which can be viewed for any case note record on the Case Notes screen. This date is generally the date on which a patient was seen by a counselor or therapist, either for group or individual counseling. However it is possible that a billable case note type can be entered for a date on which a patient was not interacted with.
(Dosing) Both: This service applies to both window and takeout doses administered. These charges are created at the time a dosing transaction is recorded on the Dose Patient screen. The rate(s) charged will be the same for both window and takeout doses administered, on a Per-Daily-Dose basis, meaning that if the patient is a split-doser, the patient is only charged once for the day regardless of the number of split-doses administered.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines varies depending on the 'Service Line Policy' selection made for the service (see the 'Service Line Policy' field description below), as follows:
Per Charge: The DoS is the date on which the dosing transaction was entered on the Dose Patient screen, regardless of how many doses the patient received, and which can be viewed for any dosing transaction on the Dosing History screen. For example, a patient receiving 1 Window dose and 6 takeout doses will have 1 charge generated, and subsequently one service line with one DoS date.
Per Transaction: A separate service line and DoS will be generated for each dose when claims are generated, regardless of only one charge appearing on the patient's Balance Journal for the dosing transaction. Each dose's DoS is the date on which each dose is intended to be ingested by the patient. For example, a patient receiving 1 Window dose and 6 takeout doses will have 1 charge generated, and subsequently 7 service lines, one for each daily dose administered with separate, unique DoS dates for each.
Summary: The DoS date range for the generated service line will correspond exactly with the date range being used to generate claims on the Claims Generator screen, provided that the patient received a dose for the 'From Date' and 'To Date' selected. Otherwise, if the patient received any doses during the date range selected on Claims Generator, the resulting service line will have a DoS date range covering the earliest date for which the patient received a dose through the last date for which the patient received a dose. For example, if during the month of November a patient only dosed on November 8 and received a window dose and 6 takeout doses, and claims are generated for the month of November, then for this patient, one service line would be generated, with a DoS date range covering 11/8 through 11/14.
Summary Break on Absent: This Service Line Policy works very similarly to the 'Summary' Service Line Policy, except that it accounts for absenteeism and excludes absent dates from DoS date ranges by generating multiple service lines as needed. The DoS date range for the generated service line will correspond exactly with the date range being used to generate claims on the Claims Generator screen, provided that the patient received a dose for the 'From Date' and 'To Date' selected and was not absent during this period. If the patient was absent for date during the period for which claims are being generated, then the first service line generated will end with a DoS for the date prior to the absence, and generate a new service line with a DoS date range beginning on the date the patient returned to the facility. For example, if during the month of November a patient who is required to dose every day began dosing on November 8, then dosed daily through November 21, then was absent on November 22, and then was discharged after dosing on November 26th, and claims are generated for the month of November, then for this patient, two service lines would be generated. The first would have a DoS date range covering 11/8 through 11/21. The second would have a DoS date range covering 11/23 - 11/26.
(Dosing) Window Only: This service applies to only window doses administered. These charges are created at the time a dosing transaction is recorded on the Dose Patient screen. The rate(s) charged will be charged on a Per-Daily-Dose basis, meaning that if the patient is a split-doser, the patient is only charged once for the day regardless of the number of split-doses administered. The most common reason this type of service is used is for charging a different amount for window doses than takeout doses, generally for facilities submitting claims to Payers who pay different amounts for each type of dose.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines varies depending on the 'Service Line Policy' selection made for the service (see the 'Service Line Policy' field description below), as laid out above for the (Dosing) Both billable service. However, there is a key difference for this type of service because since the amount(s) being charged for a window dose is different than the amount(s) being charged for takeout dose(s), if a patient receives one or more takeout(s), then the patient will be charged twice - once for the window dose and once for the takeout dose(s). These separate charges can be viewed on the Balance Journal screen. Otherwise the same Service Line Policy rules laid out above operate the same for this type of service as it does for the Dosing (Both) service.
(Dosing) T/O Only: This service applies to only takeout doses administered. These charges are created at the time a dosing transaction is recorded on the Dose Patient screen. The rate(s) charged will be charged on a Per-Daily-Dose basis, meaning that if the patient is a split-doser, the patient is only charged once for the day regardless of the number of split-doses administered. The most common reason this type of service is used is for charging a different amount for window doses than takeout doses, generally for facilities submitting claims to Payers who pay different amounts for each type of dose.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines varies depending on the 'Service Line Policy' selection made for the service (see the 'Service Line Policy' field description below), as laid out above for the (Dosing) Both billable service. However, there is a key difference for this type of service because since the amount(s) being charged for (a) takeout dose(s) is/are different than the amount(s) being charged for a window dose, if a patient receives one or more takeout(s), then the patient will be charged twice - once for the window dose and once for the takeout dose(s). These separate charges can be viewed on the Balance Journal screen. Otherwise the same Service Line Policy rules laid out above operate the same for this type of service as it does for the Dosing (Both) service.
(Drug Screens) Acceptable: This service applies only to the drug screen test results entered or automatically downloaded into Methasoft that are deemed 'Acceptable' (clean/passing) by your facility (as configured in your database). The charge will be created at the time the drug screen test result is saved on the Drug Screen Results screen or when the drug screen test result is automatically downloaded by nightly processes.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines is the 'Test Date', which can be viewed for any drug screen test result record on the Drug Screen Results screen. This date is the date on which a patient provided a specimen to be tested for the presence or absence of drugs.
(Drug Screens) Unacceptable: This service applies only to the drug screen test results entered or automatically downloaded into Methasoft that are deemed 'Unacceptable' (dirty/failing) by your facility (as configured in your database). The charge will be created at the time the drug screen test result is saved on the Drug Screen Results screen or when the drug screen test result is automatically downloaded by nightly processes.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines is the 'Test Date', which can be viewed for any drug screen test result record on the Drug Screen Results screen. This date is the date on which a patient provided a specimen to be tested for the presence or absence of drugs.
(Scheduled Events) (Scheduled Event Name): This service applies only to the selected scheduled event. Only scheduled events marked as 'Third Party Billable?' (checked) on the Scheduler - Preferences window (launched via the Administration menu item) will be available for selection in this field. The charge will be created at the time the selected scheduled event is marked as 'Complete' (or updated with a 'Complete' status) via several different screens throughout Methasoft.
***Date of Service (DoS): If claims are generated based on these charges, the Date(s) of Service that will appear for corresponding service lines correspond to the 'Start Due Date' and 'End Due Date' of the event, which can be viewed for any scheduled event record on several screens throughout Methasoft, including the Scheduler - Calendar and Scheduler - Review Events screens. Generally this date range covers only one date, and is generally the date on which a patient is scheduled to complete a specific task. However we have seen specific types of events are scheduled to span multiple days.
(Unmanaged) (Dosing Periodic): This service is the most commonly used Unmanaged - Service Type, because it allows facilities to charge patients periodically for Dosing services based on 'Charge Option' and/or 'Charge Day' settings. 'Dosing Periodic' is the only 'Service Type' selection available that will enable the 'Charge Option' field for selecting how you want patients to be charged periodically. Note that these settings can be overridden for a specific patient on the Billable Service Overrides screen. There are 6 different charge options available, as described below:
Per Dose: Do not select this option for an Unmanaged billable service. Instead, change the selection made in the 'Billable Service' field to 'Dosing'.
Per Week: Select this 'Charge Option' if you want your patients charged each week on the Weekly Charge Day of your choosing. The charge will be created accordingly by nightly processes.
Per Month: Select this 'Charge Option' if you want your patients charged each month on the Monthly Charge Day of your choosing. The charge will be created accordingly by nightly processes.
Semi-Monthly: Select this 'Charge Option' if you want your patients charged on the 1st and 15th of each month. The charge will be created accordingly by nightly processes.
4x Monthly (Mon): Select this 'Charge Option' if you want your patients charged each month but only on the first 4 Mondays of each month, since some months contain 5 Mondays. The charge will be created accordingly by nightly processes.
Daily Encounter: Select this 'Charge Option' only if you have selected any of the 3 'Service Types' other than 'Dosing Periodic' (described below) while setting up an Unmanaged billable service.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service that will appear for corresponding service lines correspond to the nature of the 'Charge Option' selected, as described below:
Per Week: The Date of Service date range will begin on the date of the charge and end 7 days later.
Per Month: The Date of Service date range will begin on the date of the charge and end on the final day of each month for each charge.
Semi-Monthly: The Date of Service date range will begin on the first day of each month and end on the 14th day of each month for the 'first half' service line, and will begin on the 15th of each month and end on the last day of each month for the 'second half' service line.
4x Monthly (Mon): The Date of Service date range will behave just as it does for the 'Per Week' option described above, except for months which include 5 Mondays, during which no charge is even created on the 5th Monday of that month - thus no service line would be generated for that final week extending into the subsequent month.
(Unmanaged) (Daily Periodic Dosing Encounter): This service type is rarely used to accommodate specific third party payer billing requirements. This type of service only charges a patient if the patient appeared at the facility and received one or more doses of medication. The charge is created by nightly processes each evening, by checking to see whether or not the patient has a dosing transaction recorded in the system for that day.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service date range will encompass only one date, the date of the charge.
(Unmanaged) (Daily Periodic Dosing or Counselor Encounter): This service type is rarely used to accommodate specific third party payer billing requirements. This type of service only charges a patient if the patient appeared at the facility and received one or more doses of medication, or if the patient had a billable case note entered. The charge is created by nightly processes each evening, by checking to see whether or not the patient dosed that day, or had a case note entered with an entered 'Note Date' for that day.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service date range will encompass only one date, the date of the charge.
(Unmanaged) (Dosing Periodic - Has Window Dose): This service type is rarely used to accommodate specific third party payer billing requirements. This type of service only charges a patient if the patient appeared at the facility and ingested a dose of medication at the window, since it is possible for a patient to receive medication from a facility in takeout form only (for example, a Returned Early exception to pick up more takout doses). The charge is created by nightly processes each evening, by checking to see whether or not the patient has a dosing transaction recorded in the system for that day, and was specifically administered a window dose.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service date range will encompass only one date, the date of the charge.
(Unmanaged) (Dosing Periodic - T/O Only Dosing Encounter): This service type is rarely used to accommodate specific third party payer billing requirements. This Service Type allows for the generation of a periodic charge for any date on which a patient received 1 or more takeout doses, regardless of whether or not the patient received a window dose.
***Date of Service (DoS): If claims are generated based on these charges, the Date of Service date range will encompass only one date, the date of the charge.
Service Line Policy
This field is used for selecting the Service Line Policy that will govern service line generation for the billable service being entered, for facilities using the Claims Generator screen to generate claims and service lines. This field is very important for facilities submitting claims to third party payers, because often payers have specific requirements in regards to the number of service lines per claim allowed (defined on the Payer/Rate Groups screen) and/or how Dates of Service (DoS) should appear for each service line submitted. This field is only enabled to allow a selection to be made for 'Dosing' billable services, as discussed in detail above for selections made in the 'Service Type' field. The same detailed information is presented below:
***Date of Service (DoS): If claims are generated based on Dosing billable service charges, the Dates of Service that will appear for corresponding service lines vary depending on the 'Service Line Policy' selection made for the service as follows:
Per Charge: The DoS is the date on which the dosing transaction was entered on the Dose Patient screen, regardless of how many doses the patient received, and which can be viewed for any dosing transaction on the Dosing History screen. For example, a patient receiving 1 Window dose and 6 takeout doses will have 1 charge generated, and subsequently one service line with one DoS date.
Per Transaction: A separate service line and DoS will be generated for each dose when claims are generated, regardless of only one charge appearing on the patient's Balance Journal for the dosing transaction. Each dose's DoS is the date on which each dose is intended to be ingested by the patient. For example, a patient receiving 1 Window dose and 6 takeout doses will have 1 charge generated, and subsequently 7 service lines, one for each daily dose administered with separate, unique DoS dates for each.
Summary: The DoS date range for the generated service line will correspond exactly with the date range being used to generate claims on the Claims Generator screen, provided that the patient received a dose for the 'From Date' and 'To Date' selected. Otherwise, if the patient received any doses during the date range selected on Claims Generator, the resulting service line will have a DoS date range covering the earliest date for which the patient received a dose through the last date for which the patient received a dose. For example, if during the month of November a patient only dosed on November 8 and received a window dose and 6 takeout doses, and claims are generated for the month of November, then for this patient, one service line would be generated, with a DoS date range covering 11/8 through 11/14.
Summary Break on Absent: This Service Line Policy works very similarly to the 'Summary' Service Line Policy, except that it accounts for absenteeism and excludes absent dates from DoS date ranges by generating multiple service lines as needed. The DoS date range for the generated service line will correspond exactly with the date range being used to generate claims on the Claims Generator screen, provided that the patient received a dose for the 'From Date' and 'To Date' selected and was not absent during this period. If the patient was absent for date during the period for which claims are being generated, then the first service line generated will end with a DoS for the date prior to the absence, and generate a new service line with a DoS date range beginning on the date the patient returned to the facility. For example, if during the month of November a patient who is required to dose every day began dosing on November 8, then dosed daily through November 21, then was absent on November 22, and then was discharged after dosing on November 26th, and claims are generated for the month of November, then for this patient, two service lines would be generated. The first would have a DoS date range covering 11/8 through 11/21. The second would have a DoS date range covering 11/23 - 11/26.
Rendering Provider Type
This field can be used for selecting the type of rendering provider the service will associate with generated claims and service lines. If 'Entered By' is selected in this field, then the 'Rendering Provider' field will be disabled and the user who enters the record for the service provided will be automatically stored as the rendering provider for that service when claims are generated (but only if the Methasoft User is associated with a Rendering Provider record - see 'Considerations' section below). If 'Specific Provider' is selected in this field, then the specific 'Rendering Provider' can be selected, and this provider will always be automatically stored as the rendering provider for that service when claims are generated.
Rendering Provider
This field is only enabled if 'Specific Provider' is selected as the 'Rendering Provider Type' in the field above it. If 'Specific Provider' is selected as the 'Rendering Provider Type', this field is used to select the specific rendering provider for the service being configured. The list of available rendering providers is populated by all rendering providers entered on the Rendering Providers screen. All claims and service lines generated for this service on the Claims Generator screen will be associated with the rendering provider selected, unless overridden on the Billing Service Line Management window (see 'Considerations' section below).
Claim/Service Line Note
This field is used for entering the text of a claim-level (Loop 2300) or service-line level (Loop 2400) note as required by a clearinghouse and/or payer. Typically this field is not used, and thus is not required. The text entered in this field is exported to the NTE02 data element (Description) of the NTE segment (Claim Note and/or Service Line Note) in either Loop 2300 or Loop 2400. The text entered in this field can be overridden for a specific patient on the Billable Service Overrides screen in the 'Note Text' field.
Diagnosis Code
This field is used to select the primary diagnosis code to be associated with the service being entered. A selection must be made in this field if your facility is generating claims for billing export, because it is required data on billing export files. The value selected in this field is exported to the HI01 - 2 sub-element (Industry Code) of the HI01 data element (Health Care Code Information) of the HI segment (Health Care Diagnosis Code) in either Loop 2300 or Loop 2400. The value selected here can be overridden for a specific patient on the Diagnosis Codes screen, which also supports the entry of multiple Diagnosis Codes (Secondary - Quaternary) to be associated with one or more specific billable services. The most common value selected in this field is '30401' (for ICD-9). The ICD-10 option button is there for selecting an ICD-10 code once the ICD-10 mandate becomes effective.
Proc. Modifier
This field is rarely used, but is used for entering a procedure modifier for the service being configured if required by a clearinghouse and/or payer. The alphanumeric text entered in this field is exported to the SV101 - 3 sub-element (Procedure Modifier) of the SV101 data element (Composite Medical Procedure ID) of the SV1 segment (Professional Service) in Loop 2400.
Procedure Code
This field must be used by any facility submitting billing export files to payers for claim reimbursement, but is optional for all other facilities. The alphanumeric text (generally a 5-digit code) entered in this field is exported to the SV101 - 2 sub-element (Product/Service ID) of the SV101 data element (Composite Medical Procedure ID) of the SV1 segment (Professional Service) in Loop 2400.
Service Facility
This field is used for selecting the service facility where the billable service is being rendered. The list of service facilities available for selection is populated by all service facilities entered on the Service Facilities screen. Generally there is only one available selection in this field, which is your facility. All claims and service lines generated for this service on the Claims Generator screen will be associated with the service facility selected.
Payer Rate
This field is used to define the amount of money that the Third Party Balance of a patient will be charged each time a billable service is rendered. For 'Counseling' services, this field is used to define the amount of money to be charged for each billable unit of the counseling service being rendered, which depends on the definition of one unit of counseling at your facility, as defined in Counselor Preferences and/or on the Case Note Templates screen.
Patient Rate
This field is used to define the amount of money that the Patient Balance of a patient will be charged each time a billable service is rendered. For 'Counseling' services, this field is used to define the amount of money to be charged for each billable unit of the counseling service being rendered, which depends on the definition of one unit of counseling at your facility, as defined in Counselor Preferences and/or on the Case Note Templates screen.
Include Patient Responsibility In Claim
This field is currently disabled and is not being used.
Note Qualifier
This field is used for selecting the qualifier type of a claim-level (Loop 2300) or service-line level (Loop 2400) note as required by a clearinghouse and/or payer. Typically this field is not used, and thus is not required. The value selected in this field is exported to the NTE01 data element (Note Reference Code) of the NTE segment (Claim Note and/or Service Line Note) in either Loop 2300 or Loop 2400. The value selected in this field can be overridden for a specific patient on the Billable Service Overrides screen in the 'Note Type Qualifier' field.
Copay Amount
This field is currently disabled and is not being used.
Per Visit Copay
This field is currently disabled and is not being used.
Charge Option
This field only becomes enabled if 'Unmanaged' is selected in the 'Billable Service' field, and should only be used if 'Dosing Periodic' is selected in the 'Service Type' field. As detailed above for the Unmanaged - Dosing Periodic billable service type, the available selections in this field function as described below:
Per Dose: Do not select this option for an Unmanaged billable service. Instead, change the selection made in the 'Billable Service' field to 'Dosing'.
Per Week: Select this 'Charge Option' if you want your patients charged each week on the Weekly Charge Day of your choosing. The charge will be created accordingly by nightly processes.
Per Month: Select this 'Charge Option' if you want your patients charged each month on the Monthly Charge Day of your choosing. The charge will be created accordingly by nightly processes.
Semi-Monthly: Select this 'Charge Option' if you want your patients charged on the 1st and 15th of each month. The charge will be created accordingly by nightly processes.
4x Monthly (Mon): Select this 'Charge Option' if you want your patients charged each month but only on the first 4 Mondays of each month, since some months contain 5 Mondays. The charge will be created accordingly by nightly processes.
Daily Encounter: Select this 'Charge Option' only if you have selected any of the 3 'Service Types' other than 'Dosing Periodic' (described below) while setting up an Unmanaged billable service.
Wkly Chrg Day / Mnthly Chrg Day
This field only becomes visible if 'Per Week' or 'Per Month' is selected in the 'Charge Option' field above it, and is named differently accordingly. It is used to select the day of the week or month on which your facility wishes to charge patients for an Unmanaged - Dosing Periodic billable service. The charge is created by nightly processes based on the day of week or month selected. The data entered/selected in this field can be overridden for specific patients on the Billable Service Overrides screen.
Effective On
This field is used for selecting the date on which the entered billable service takes effect, or begins to create charges.
Effective To
Generally this field is left blank, so that the service remains effective indefinitely. However, when scheduling a rate change for example, this field is used for selecting the date on which a billable service is no longer in effect, or the last day that it will create charges. A facility might also set the Effective To date to a future date if they know, for example, that a Payer is no longer going to reimburse them for services as of a specific date, so that Methasoft will stop charging patient third party balances after the entered date.
Payer/Rate Group
This column displays the 'Payer/Rate Group' selected to be associated each billable service.
Billable Service Name
This column displays the name of each billable service as entered in the 'Service Name' field.
Service
This column displays the 'Billable Service' selected for each billable service.
Service Type
This column displays the type of service selected in the 'Service Type' field for each billable service.
Effective On
This column displays the date selected/entered in the 'Effective Date' field for each billable service, indicating when the service will begin to create charges.
Effective To
This column displays the date selected/entered in the 'Effective Date' field for each billable service, which is generally left blank (open-ended/indefinite), indicating the last date on which the service will create charges.
Payer
This column displays the amount in US dollars entered in the 'Payer Rate' field, indicating the amount Third Party Balances will be charged for each billable service.
Patient
This column displays the amount in US dollars entered in the 'Patient Rate' field, indicating the amount Patient Balances will be charged for each billable service.
More...
After selecting a billable service on the grid, pressing this button launches the Billable Service Additional Information window shown below, where additional settings can be configured for each Billable Service.
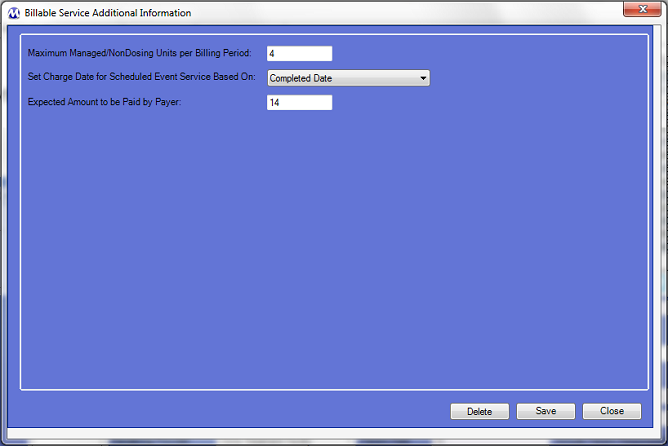
Currently there are only 3 additional settings, described below:
Maximum Managed/NonDosing Units per Billing Period
Setting a value in this field can help prevent users from accidentally over-charging for Managed/Non-Dosing billable services. Normally this value is left blank, but can be useful in facilities trying to prevent, for example, erroneous Case Note record entries entered with a higher number of Billable Units than is appropriate.
Set Charge Date for Scheduled Event Service Based On:
This field applies only to Scheduled Event services, and only 2 options are available in this field:
Completed Date - If this option is selected, then the Charge Date saved for a Scheduled Event service charge will be the date on which the associated Scheduled Event is Completed (has its Status updated to 'Complete') in Methasoft, which is also the time at which the charge will be generated in Methasoft.
Scheduled Date - If this option is selected, then the Charge Date saved for a Scheduled Event service charge will be the 'Start Due Date' of the associated Scheduled Event. The charge will be generated in Methasoft at the time at which the Scheduled Event is Completed (has its Status updated to 'Complete').
Expected Amount to be Paid by Payer:
This field applies to the Payer Rate field of the selected Billable Service. It is the amount a facility actually expects to be paid for a rendered service from a third party Payer, regardless of the amount claimed for the service. This value can be useful for determining 'projected revenue' based on the amount a facility expects to be paid for a rendered service as opposed to using the amount being claimed.
Pressing this button runs and prints the Billable Services report to your configured printer, listing all Billable Services entered on this screen.
Dosing Billable Services Must be Configured on this Screen Prior to Using the Basic Charge Dosing Information Screen
In order for a Payer/Rate Group to appear available for selection on the Basic Dosing Charge Information screen grid, a Dosing or Unmanaged billable service must be entered and associated with that Payer/Rate Group.
Required Fields - Self Pay-Only Facilities and/or Third Party Billing Facilities
Because quite a few fields on this screen pertain only to facilities generating claims and/or exporting medical billing files, we tried to minimize the number of required fields for efficiency in Self Pay-Only facilities. So if your facility is using Methasoft to generate claims and/or export billing files, it's important to evaluate each field on this screen and enter data in each as mandated by your clearinghouse and/or payer, regardless of whether or not Methasoft requires it.
Using Additional Charges on Patient Payments Instead of Scheduled Event Billable Services
Many facilities regularly our Additional Charge functionality on the Patient Payments screen to charge Patient and/or Third Party Balances for additional items, including 'services'. In light of the new Accounting/Billing functionality released in Methasoft Version 6, each facility should consider which route to take going forward, in terms of charging for these items or services. If for example, your facility has always wanted to generate claims for additional charges and previously couldn't, your facility now has an option by which to do so via Scheduled Event billable services or one of the new Billable Services available, such as Drug Screens or Absences. We have been and are evaluating the possibility of creating a new Billable Service type called 'Additional Charges' for integration with the old Additional Charge functionality, however at this point in time it cannot be predicted if or when such a service type might be available.
Understanding How to Use 'Unmanaged' Billable Services, Related Service Types, and Charge Options
It's very important to read the detailed Field Descriptions above in regards to Unmanaged services to fully understand how they function and why we created them. We use the term 'Managed' when describing a service that creates a charge that is stored with a direct association to another system transaction, such as a dosing transaction entered on the Dose Patient screen. We use the term 'Unmanaged' when describing a service that creates a charge that is not stored with a direct association to any other system transaction, but rather charges on the basis of the passage of time alone (periodically).
Editing or Deleting Billable Services
Methasoft attempts to cover as many scenarios as possible to prevent users from creating bad data, or losing data, inadvertently by editing or deleting a Billable Service that is currently in use or has been previously associated with generated charges and/or claims. However users should use caution and really think through the change being made, particularly in regards to which fields are being affected (of course Deleting a service affects the entire service record, and thus all fields). For example, editing the name of a Billable Service is unlikely to cause any real harm (though it could cause a temporary headache for other users if the change is not communicated properly). Whereas, for example, editing the Effective date range of a billable service could potentially cause a wide range of problems which cannot be quickly fixed. If you are uncertain about the ramifications of editing or deleting a Billable Service, please confirm what you are about to do internally with someone at your facility, or contact Methasoft Customer Support prior to editing or deleting the Billable Service.
Editing or Deleting Billable Services for Third Party Billing - Potential Timing/Workflow Issues Related to Claim Generation/Billing Export
Related to the Consideration above this one, when editing a Billable Service for which claims are being exported, it is important to consider the timing of the edit. For example, some data entered on this screen is retrieved at the time of exporting generated Claims. Thus, if Claims have already been exported but not yet submitted to a Payer, it is generally a good rule of thumb to edit the Billable Service data then re-export the unsubmitted Claims. All staff responsible for billing activities within a facility should make sure they understand the billing workflow within their facility, and communicate changes that are being made in Methasoft accordingly, in order to minimize billing export file rejection. Similar examples apply to the timing of claim generation, along with the timing of export file generation and/or submission. And all of these principles apply when deleting a Billable Service, even more than when editing a service.
Billable Service and Billing Episode Date Ranges
In order for a patient's Third Party and/or Patient balance to be charged for a rendered service, the patient must have a current/effective Billing Episode associated with a Payer/Rate Group that is associated with one or more current/effective Billable Services. In both cases, this is determined by the Effective date ranges of each. We advocate using open-ended/indefinite Billing Episode and Billable Service date ranges as much as possible, meaning the Expiration Date of Billing Episodes should be left blank as often as possible, and the Effective To date of Billable Services should be left blank as often as possible. The Missing Charges report was added to Methasoft to help customers find charges that should be in the system but are not - 99% of the time, the missing charges were the result of changes made to the Effective date range of either a Billing Episode or a Billable Service by a user who was unaware of the ramifications of their changes.
The Billable Service Overrides Screen
The Billable Services Overrides Screen provides users with a way to override global Billable Service settings, as defined on this screen, for a specific patient. This feature is most commonly used to accommodate highly unusual circumstances, such as a one-off unusual attendance schedule for a specific patient. We advise facilities to use the Billable Service Override screen as little as possible, because when over-used it defeats the purpose of much of the enhanced functionality added for Methasoft Version 6. Furthermore, the service override data must be entered precisely to match the billable service data being overridden or it will not charge the patient properly - in many facilities this can cause a problem because a user does not have access to the Billable Services screen to verify that the override record being entered accurately matches the service being overridden. While the Billable Service Overrides screen is a powerful feature to accommodate unusual circumstances, we recommend that it should be used very carefully and as sparingly as possible.
The Diagnosis Codes Screen
The Diagnosis Codes screen can be used to override the Primary Diagnosis Code selected for a Billable Service, as well as add additional diagnosis codes (secondary - quaternary) for a specific patient. In facilities submitting generated claims, using this screen is sometimes necessary in order for a patient's claim to be paid, depending on specific payer requirements.
The Importance of Associating Methasoft Users with Rendering Providers for 'Entered By' Rendering Provider Type Services
It's important for a facility's staff to maintain the habit of associating Methasoft users with Rendering Provider records when applicable, at the time at which the user's Employee Profile is created in combined with the creation of their new Rendering Provider record. This association is made by using the Billing Assoc. button on on the Employee Profile screen once an Employee Profile has been created. This only matters if your facility is using Billable Services using the 'Entered By' Rendering Provider Type, in which case a user trying to generate claims can run into the problematic scenario of being unable to do so because one or more associations have not been established, and then is unable to access the Employee Profile screen in order to fix the issue. The Claims Generator screen does identify this problem specifically if it's encountered at the time of claim generation.
Overriding Billable Service Data on the Billing Service Line Management Window
On the Claims Generator screen, there is a button at the bottom called Edit Service Lines which can be used to open the Billing Service Line Management window, where users can override some service line data. This window was created to accommodate rare and unusual circumstances. We recommend that it be used as little as possible, because when it's used to override service line data, often confusion will result later because the data, for example, coming back on documents from a Payer may not match, for example, the Billable Service data in Methasoft which was overridden. If a facility's Payer/Rate Groups, Billable Services and Billing Episodes are configured properly, then the need to edit service line data should be very rare if not avoided entirely.
Using Billable Services to Charge for Scheduled Events
Workflow at your facility is critical to successfully using Scheduled Event Billable Services, because these services do not create a charge until the event is completed (or the event status is updated to 'Complete'), which means someone has to be responsible for completing the event. This is not a problem as long as a facility's staff clearly understands the process and who is responsible for completing scheduled events within appropriate time frames. If events are not completed within appropriate time frames, then patients will not be charged, which could not only cost the facility a great deal of money, but could also disrupt the third party billing workflow of other staff members who are counting on scheduled events to be completed within appropriate time frames, resulting in claims that are missing service lines.
Using Billable Services to Charge for Scheduled Events with More Than One Attendee
As a general rule of thumb, we do not recommend scheduling more than one attendee for a scheduled event associated with a billable service. The reason why is because it's too common for one or more attendees to not complete the task, and if the event cannot be fully completed, then no charges will be created for any of the attendees. If a facility goes against this recommendation, someone at the facility will have to really stay on top of the appropriate completion of scheduled events, as well as manage such event attendee lists in light of discharges, intakes, absenteeism, incarceration, guest-dosing, etc..., on a daily basis. From our perspective this is unnecessary and should be avoided.
Using Counseling Billable Services - Units, Rates and Case Note Templates
Before configuring Billable Services for Counseling on this screen, it's very important that you have the appropriate 'Default Time increment for billable units' Preference value set (see 'Related Preferences' below) and/or all of your Case Note Templates configured properly, because this service type charges the defined Payer and/or Patient Rates PER UNIT, as entered in the 'Billable Units' field on the Case Notes screen when a billable case note is saved. The most common way to prevent overcharging for Counseling services is to use the functionality available on the Case Note Templates screen to define specified numbers of units per note type and/or lock-down the 'Billable Units' field so that users cannot change that value.
Using Drug Screen Billable Services - Editing or Deleting Drug Screen Results Does Not Fix Associated Charges
If you are using Billable Services to create charges for Drug Screens, be aware that once a drug screen charge has been created, it will not change if the underlying drug screen date is changed, or if the underlying drug screen is deleted. This means that if a drug screen date must be edited, or if a drug screen result must be deleted, and a charge already exists for this drug screen, the charge must also be deleted. If the underlying drug screen date was edited, then the charge must be regenerated following the drug screen date edit.
Resulting Dates of Service (DoS) for Generated Service Lines - Always a Date Range Even if Only One Date is Covered
When Claims are generated in Methasoft, each Service Line uses a date range to define the Date(s) of Service, even if the Date of Service is only one day, in which case the date range will start and end on the same date. This is handled properly when electronic billing export files are generated and thus should not be a source of concern. Service Line functionality must work this way given the wide range of services which require a multi-day date range for the Dates of Service data to be accepted by payers.
Basic Dosing Charge Information
Diagnosis Codes
Claims Generator
Claims Generator - Edit Service Lines - Billing Service Line Management
Billing Export
Batch Payments
Understanding the 837 Professional (837P) Export File Format
Loop 2300 (Claim data)
Loop 2400 (Service Line data)
Troubleshooting EDI File and Claim Rejections/Denials
Payment Information (Deprecated)
Aging Claims
Batch Payments
Billable Services
Billable Units Summary by Payer
Billing Episodes Expiring
Case Notes Billable Units by Payer
Case Notes Billable Units Summary by Payer
Caseload Summary by Payer
Claims by Payer
Claims Summary
Intakes and Discharges by Modality
Missing Charges
No Show Preview Today by Counselor
Outstanding Claims
Patient and Payer Charges
Patient Insurance Eligibility
Patient List by Billing Episode
Patient List by Modality/Payer
Patient List by Payer
Patient List for Billing by Counseling Category
Patient List History by Payer
Patient Medication Record Breakdown by Payer
Patient Medication Record for Billing
Payment Information Patient Charges Dosing
Prior Authorizations
Service Checks
Service Lines by Claim
Service Lines by Service
Administration Menu - Scheduler - Preferences Window - Third Party Billable?