![]()
![]()
Basic Dosing Charge Information
(Topic Last Updated On: 03/12/2015)
The Basic Dosing Charge Information menu item on the Accounting menu launches the Basic Dosing Charge Information screen, which is used to efficiently set up how patients will be charged for Dosing (Treatment) billable services. This screen was introduced in Methasoft 6.0 to essentially replace the Payment Information screen used in previous versions, allowing users to benefit from new billing and Payer/Rate Group functionality while retaining the functionality of the Payment Information screen. This screen is only populated by configured Dosing and/or Unmanaged Billable Services, and only when such services are associated with a Payer/Rate Group with a 'Basic (Self Pay)' Validation Level. This ensures that users at facilities using Methasoft's full billing functionality are required to enter critical data on the Billing Episodes screen for patients for whom they intend to generate and/or electronically submit billing claims. However Third Party balance related fields are retained on this screen for facilities who wish to track Third Party balances for any reason without using Methasoft's full billing functionality, thereby retaining and enhancing the functionality available to users on the Payment Information screen in prior versions of Methasoft. This screen should be used by most facilities using Methasoft for efficient Dosing (Treatment) charge setup for each patient. An exception would be a facility where the vast majority of their patients are insured, and the facility is generating and/or electronically submitting billing claims for each. See the 'Considerations' section below which discusses the 4 primary facility Dosing (Treatment) charge scenarios and how this screen should be used in light of each.
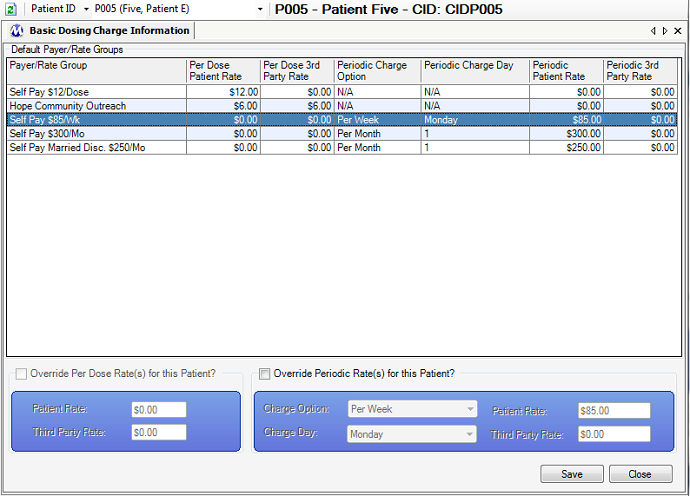
Override Per Dose Rate(s) for this Patient?
This checkbox will remain disabled unless a Dosing Billable Service is associated with the Payer/Rate Group selected on the grid. If this field is checked, then the 'Patient Rate' and 'Third Party Rate' fields below it will become enabled, allowing users to override the rate(s) charged to each Balance Type for the retrieved patient. The patient will then be charged the override rate(s) for Dosing instead of the default rate(s) defined on the Billable Services screen.
Patient Rate (Per Dose)
This field becomes enabled if the 'Override Per Dose Rate(s) for this Patient?' checkbox is checked, and the entered rate will be used to charge the patient's Patient Balance instead of the default rate defined for the associated service on the Billable Services screen.
Third Party Rate (Per Dose)
This field becomes enabled if the 'Override Per Dose Rate(s) for this Patient?' checkbox is checked, and the entered rate will be used to charge the patient's Third Party Balance instead of the default rate defined for the associated service on the Billable Services screen.
Override Periodic Rate(s) for this Patient?
This checkbox will remain disabled unless an Unmanaged Billable Service is associated with the Payer/Rate Group selected on the grid. If this field is checked, then the 'Charge Option', 'Charge Day', 'Patient Rate' and 'Third Party Rate' fields below it will become enabled, allowing users to override the frequency (Charge Option), charge day (if applicable) and/or rate(s) charged to each Balance Type for the retrieved patient. The patient will then be charged according to the override data entered instead of the default configuration defined for the associated service on the Billable Services screen.
Charge Option
This field becomes enabled if the 'Override Periodic Rate(s) for this Patient?' checkbox is checked, and the selected Charge Option will be used to charge the patient instead of the default Charge Option defined for the associated service on the Billable Services screen.
Charge Day
This field may or may not be visible depending on the 'Charge Option' selected in the field above, because it only applies to 'Per Week' or 'Per Month' charge options. When applicable, this field becomes enabled if the 'Override Periodic Rate(s) for this Patient?' checkbox is checked, and the entered day of the week or month will be used to charge the patient instead of the default Charge Day defined for the associated service on the Billable Services screen.
Patient Rate (Periodic)
This field becomes enabled if the 'Override Periodic Rate(s) for this Patient?' checkbox is checked, and the entered rate will be used to charge the patient's Patient Balance instead of the default rate defined for the associated service on the Billable Services screen.
Third Party Rate (Periodic)
This field becomes enabled if the 'Override Periodic Rate(s) for this Patient?' checkbox is checked, and the entered rate will be used to charge the patient's Third Party Balance instead of the default rate defined for the associated service on the Billable Services screen.
Payer/Rate Group
This column displays the Payer Name of each Payer/Rate Group appearing on the grid, as defined in the 'Payer Name' field on the Payer/Rate Groups screen.
Per Dose Patient Rate
If the Payer/Rate Group is associated with a Dosing Billable Service, then this column displays the rate a patient's Patient Balance will be charged for each daily dose received, as defined on the Billable Services screen. This column does not display an override rate if one is entered, but instead only the default rate as defined on the Billable Services screen. See 'Considerations' section below.
Per Dose 3rd Party Rate
If the Payer/Rate Group is associated with a Dosing Billable Service, then this column displays the rate a patient's Third Party Balance will be charged for each daily dose received, as defined on the Billable Services screen. This column does not display an override rate if one is entered, but instead only the default rate as defined on the Billable Services screen. See 'Considerations' section below.
Periodic Charge Option
If the Payer/Rate Group is associated with an Unmanaged Billable Service, then this column displays the Charge Option (frequency) being used to charge a patient periodically, based on the Charge Option (and Charge Day when applicable) selected, as defined on the Billable Services screen. This column does not display an override Charge Option if one is selected, but instead only the default Charge Option as defined on the Billable Services screen. See 'Considerations' section below.
Periodic Charge Day
If the Payer/Rate Group is associated with an Unmanaged Billable Service, then this column displays the Charge Day (when applicable) on which a patient will be charged periodically, based on the Charge Option selected, as defined on the Billable Services screen. This column does not display an override Charge Day if one is selected, but instead only the default Charge Day as defined on the Billable Services screen. See 'Considerations' section below.
Periodic Patient Rate
If the Payer/Rate Group is associated with an Unmanaged Billable Service, then this column displays the rate a patient's Patient Balance will be charged based on the Charge Option (and Charge Day when applicable) selected, as defined on the Billable Services screen. This column does not display an override rate if one is entered, but instead only the default rate as defined on the Billable Services screen. See 'Considerations' section below.
Periodic 3rd Party Rate
If the Payer/Rate Group is associated with an Unmanaged Billable Service, then this column displays the rate a patient's Third Party Balance will be charged based on the Charge Option (and Charge Day when applicable) selected, as defined on the Billable Services screen. This column does not display an override rate if one is entered, but instead only the default rate as defined on the Billable Services screen. See 'Considerations' section below.
|
***Note: There is currently no way to delete a patient's Basic Dosing Charge Information directly on this screen, because this should be a rarely used procedure. See 'Considerations' below.
1.) Retrieve the patient on the Billing Episodes screen.
2.) Select the patient's current, effective billing episode on the grid.
3.) Press the Delete button. A 'Delete this Record?' application message will appear, confirming you wish to delete the selected episode.
4.) Click on Yes to delete the billing episode or No to cancel.
5.) If an 'Override...' checkbox was selected on the Basic Dosing Charge Information screen, then that means a Billable Service Override record was created and needs to be deleted.
6.) Retrieve the patient on the Billable Service Overrides screen.
7.) Select the Billable Service Override record that matched the 'Override...' data entered on the Basic Dosing Charge Information screen.
8.) Press the Delete button. A 'Delete this Record?' application message will appear, confirming you wish to delete the selected override record.
9.) Click on Yes to delete the override record or No to cancel.
|
Data Displayed on the 'Default Payer/Rate Groups' Grid Does Not Display Override Rates
It is important for users to get used to looking at both the Payer/Rate Group grid selection as well as the 'Override...' fields below the grid, because the 'Default Payer/Rate Groups' grid does not display 'Override...' data entered for a retrieved patient. The reason for this is that we discovered it actually introduces more user confusion if the 'Override...' data is displayed on the grid for a retrieved patient than if it is not. The 'Default Payer/Rate Groups' grid will always display only the default associated Billable Service data as configured on the Billable Services screen.
Scenario 1 - Self Pay Only Facility
This the most common scenario observed in the field amongst facilities using Methasoft. The screen shot shown at the top of this topic is often how this screen might appear in a Self Pay Only facility. Once the Payer/Rate Groups and associated Billable Services are configured, this makes it very simple for these facilities to set up new patients to be charged for Dosing (Treatment).
Scenario 2 - Self Pay and/or Third Party Facility Not Using Methasoft to Generate or Export Billing Claims
Some facilities track Third Party balances for patients but do not generate or export claims using Methasoft. The most common reasons for this are that a facility uses an alternative method by which to file billing claims, or, for example, has patients with third party payers unrelated to health insurance. In the screen shot presented at the top of this topic a hypothetical example of this latter scenario is shown - the 'Hope Community Outreach' payer/rate group, which is configured to charge an assigned patient's Patient Balance $6 Per Dose and Third Party Balance $6 Per Dose. This is intended to represent a charitable Third Party organization that subsidizes a patient's treatment costs. However, for this scenario, a user might also see numerous health insurers listed on this screen - there's nothing wrong with that at all, provided the facility is using minimal billing functionality within Methasoft. The data a facility wants stored in Methasoft is critical in determining how Payer/Rate Groups and Billable Services should be configured for use on this screen, and/or the Billing Episodes screen and/or the Billable Service Overrides screen.
Scenario 3 - Self Pay / Third Party Facility Using Methasoft to Generate or Export Billing Claims
In this scenario, accounting / billing users will need to understand when to use this screen as opposed to the Billing Episodes and Billable Service Overrides screens. As a general rule of thumb, in this facility the Basic Dosing Charge Information screen should be used for Self Pay patients, but the Billing Episodes and Billable Service Overrides screen should be used for Third Party billing patients for whom claims are being generated.
Scenario 4 - Third Party Only Facility Using Methasoft to Generate or Export Billing Claims
In this scenario it is advised to always use the Billing Episodes and Billable Service Overrides screen, to ensure the necessary billing claim data is stored in Methasoft for billing claims to be accepted and paid on.
Billing Episode Records - Automatically Inserted / Updated
This consideration pertains to Considerations and the Delete procedure shown above. When a patient's Basic Dosing Charge Information is saved or edited, behind the scenes this creates or modifies the patient's current, effective Billing Episode. This Billing Episode record can be viewed on the Billing Episodes screen at any time, however many facilities will have no need to even think about this record nor ever need to access the Billing Episodes screen (particularly Self Pay-Only facilities). It is important for each facility to clearly define their internal accounting / billing procedures for handling how this functionality works, because it can become confusing, for example, if a patient is constantly bouncing back and forth between being Self Pay and being covered by health insurance (for this example, we would recommend solely using the Billing Episodes screen for this patient).
Billable Service Override Records - Automatically Inserted / Updated
This consideration pertains to Considerations and the Delete procedure shown above. When a patient's Basic Dosing Charge Information is saved or edited and 'Override...' data has been entered, behind the scenes this creates or modifies a Billable Service Override record for the patient, which is associated with the patient's current, effective Billing Episode. This Billable Service Override record can be viewed on the Billable Service Overrides screen at any time, however many facilities will have no need to even think about this record nor ever need to access the Billable Service Overrides screen (particularly Self Pay-Only facilities). It is important for facilities to be aware of this functionality, and ensure that override records are cleaned up appropriately as described at the end of the Delete procedure above. Currently Methasoft does not delete Billable Service Override records when an associated Billing Episode is deleted.
Billable Service Override Records - Using Them Should Be Minimized as Much as Possible
This consideration is also covered in the Payer/Rate Group, Billable Services, and Billable Service Overrides topics because it can't be emphasized enough. There are fairly rare scenarios where using overrides makes sense, because when override records are used, then some of the primary benefits of Payer/Rate Group functionality is lost. The most common example is when a facility needs to change service rates for hundreds of patients. If hundreds of patients have override records, then accomplishing this will be very time-consuming if the rates needs to be changed for these patients. Whereas if they are assigned to Payer/Rate Groups without override records, the rate change can be accomplished quite quickly via the Billable Services screen, without the need to retrieve hundreds of patients one-at-a-time on the Billable Service Overrides and/or Basic Dosing Charge Information screens. There are additional considerations as well depending on many different possible accounting / billing scenarios a facility might accommodate.
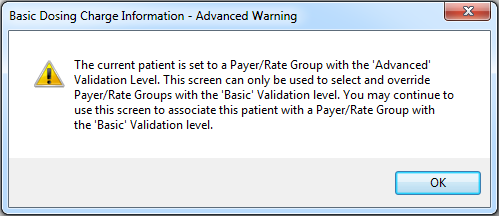
The Basic Dosing Charge Information - Advanced Warning Window
This pop-up window is displayed below, and appears if a patient who has a current/effective Billing Episode associated with a Payer/Rate Group that has a Validation Level set to 'Advanced' is retrieved on the Basic Dosing Charge Information screen. This pop-up window is designed to remind the user that if the user proceeds to save the retrieved patient to a Payer/Rate Group selected on the Basic Dosing Charge Information screen, that doing so will end the patient's current Billing Episode and create a new one associated with the Payer/Rate Group selected. Often this is exactly what the user would like to do, in which case pressing the Ok button will allow the user to proceed. However sometimes the wrong patient is accidentally retrieved on the Basic Dosing Charge Information screen, in which case after pressing the Ok button on this message, the user needs to retrieve the correct patient or close the Basic Dosing Change Information screen without saving any changes.
The Importance of Thinking Through Payer/Rate Group and Billable Service Configuration to Best Fit Your Facility's Needs
This topic again underscores the importance of each facility really thinking through the best Payer/Rate Group - Billable Service configuration to accommodate the facility's accounting / billing needs. We've observed that proper configuration and procedural establishment up-front can save a facility numerous headaches and wasted time down the road.
Billable Services
Billable Units Summary by Payer
Billing Episodes Expiring
Missing Charges
Patient and Payer Charges
Patient List by Billing Episode
Patient List by Modality/Payer
Patient List by Payer
Patient List History by Payer
Patient Medication Record Breakdown by Payer
Patient Medication Record for Billing
Payment Information Patient Charges Dosing
Automatically insert default Payment Information on new patients
Default payer when assigned automatically