![]()
![]()
(Topic Last Updated On: 06/08/2015)
The Billable Service Overrides menu item on the Accounting menu launches the Billable Service Overrides screen, which is used to override Billable Service data for a specific patient so that the patient is charged differently than the associated Billable Service being overridden. A Billable Service Override record is associated with a patient's specific Billing Episode, which allows multiple records to be entered on this screen if necessary to accommodate Billing Episode changes and charge re-generation scenarios. Though we recommend using this screen as little as possible, it provides the functionality necessary to accommodate unusual scenarios for specific patients, such as charging a patient a different rate, or charging them on a different date for services rendered. Methasoft automatically validates whether or not the Billable Service Override record entered is valid by checking configured Billable Services to ensure that the specific type of Billable Service selected exists. If the underlying Billable Service type does not exist, a message appears informing the user of this and prevents the user from saving the override record. Billable Service Override functionality is integrated with the Basic Dosing Charge Information screen, so that when users enter data in the 'Override...' fields on the Basic Dosing Charge Information screen, Billable Service Override record data is automatically updated behind the scenes. Self Pay-Only facilities using the Basic Dosing Information screen generally never use the Billable Service Overrides screen. Facilities using third party billing functionality in Methasoft are encouraged to use the Billable Service Overrides screen as little as possible, and to instead take advantage of the benefits of Payer/Rate Groups by configuring more them. This screen is intended for unusual patient-specific circumstances applicable only for small groups of patients. This screen also allows facilities using third party billing functionality to override the 'Claim/Service Line Note' and/or 'Note Qualifier' defined globally on the Billable Services screen for a specific patient to accommodate unusual Clearinghouse and/or Payer requirements.
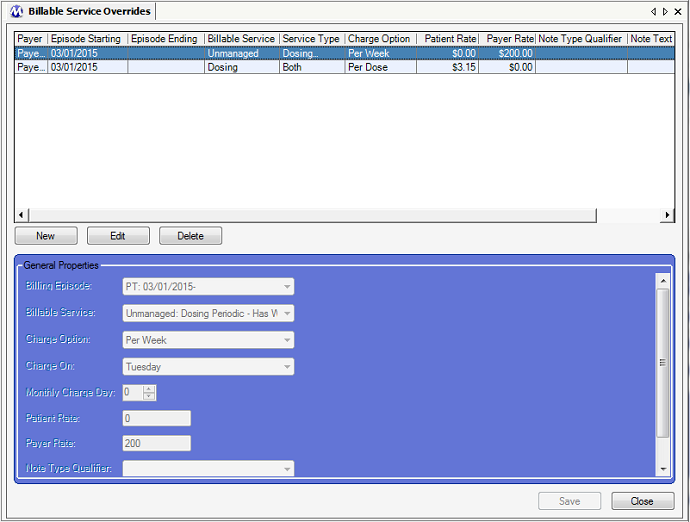
Billable Service Overrides - An Example of an Unmanaged - Dosing Periodic - Has Window Dose Override to Charge the Payer on a Different Week Day
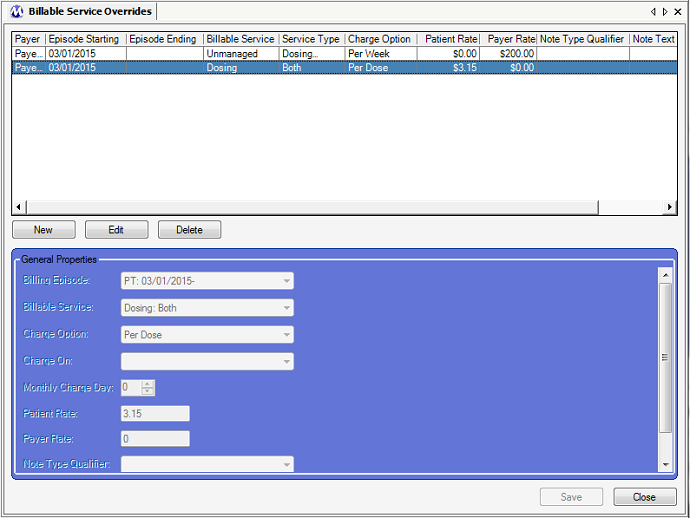
Billable Service Overrides - An Example of a Managed Dosing - Both Service Override to Charge the Patient and Payer Different Rates
Billing Episode
This field is used for selecting the specific for which the override record will apply. Once the selected billing episode ends, the override record associated with it will no longer apply except in cases where charges need to be regenerated for date ranges which include past billing episode effective dates. In other words the effective date range of the override record is the effective date range of the billing episode to which it's associated.
Billable Service
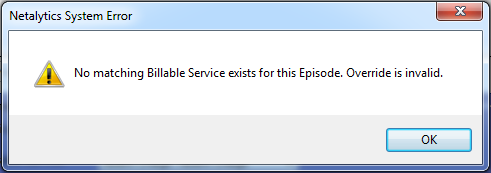
This field is used for selecting the specific billable service and service type to be overridden. Currently override records can be entered for the 'Absent Charge' service type, the 3 managed 'Dosing' service types, and the 4 unmanaged periodic 'Dosing' service types. Methasoft will not all you to save the override record unless a current/effective matching billable service type is found for the payer/rate group associated with the billing episode selected. When this occurs, the message shown below will appear, and the user will need to either adjust the selection in this field or enter a current/effective billable service on the Billable Services screen. This message prevents the entry of invalid override records which would not function.
Charge Option
This field is used to select the charge option if either a managed or unmanaged 'Dosing' or periodic 'Dosing' billable service type is selected in the 'Billable Service' field. It is important to select the appropriate charge option in this field for the billable service type selected in the 'Billable Service' field, according to the rules listed below:
If one of the 3 managed 'Dosing' service types (Dosing: Both, Dosing: T/O Only, Dosing: Window Only) is selected in the 'Billable Service' field, then 'Per Charge' must be selected in this field.
If one of the 2 unmanaged periodic 'Encounter' service types (Unmanaged: Daily Periodic Dosing Encounter, Unmanaged: Daily Periodic Dosing or Counseling Encounter) is selected, or if the 'Unmanaged: Dosing Periodic - Has Window Dose' service type is selected in the 'Billable Service' field, then 'Daily Encounter' must be selected in this field.
If 'Unmanaged - Dosing Periodic' is selected in the 'Billable Service' field, then one of the 4 periodic charge options must be selected in this field (Per Week, Per Month, Semi-Monthly, 4x/Month (Mon)).
***Note: It is common for this selection to be the same as the 'Charge Option' defined on the Billable Services screen for 'Per Week' or 'Per Month' unmanaged periodic services when a user simply wants to override the day of the week or month on which to charge a patient.
If 'Absent Charge: Absent Charge' is selected in the 'Billable Service' field, then this field can be left blank and skipped.
Charge On
This field is only used if 'Unmanaged - Dosing Periodic' is selected in the 'Billable Service' field, and 'Per Week' is selected in the 'Charge Option' field. This field is used for selecting the day of the week on which the patient will be charged.
Monthly Charge Day
This field is only used if 'Unmanaged - Dosing Periodic' is selected in the 'Billable Service' field, and 'Per Month' is selected in the 'Charge Option' field. This field is used for selecting the day of the month on which the patient will be charged.
Patient Rate
This field is used for entering the US dollar amount the patient's Patient balance will be charged for the rendered billable service type selected in the 'Billable Service' field.
***Note: It is important that a rate be entered in this field regardless of whether or not the rate is different from that defined on the Billable Services screen, because if a user wishes to override one type of rate but not the other, Methasoft will use both rates entered in the Patient Rate and Payer Rate fields to charge the patient.
Payer Rate
This field is used for entering the US dollar amount the patient's Third Party balance will be charged for the rendered billable service type selected in the 'Billable Service' field.
***Note: It is important that a rate be entered in this field regardless of whether or not the rate is different from that defined on the Billable Services screen, because if a user wishes to override one type of rate but not the other, Methasoft will use both rates entered in the Patient Rate and Payer Rate fields to charge the patient.
Note Type Qualifier
This field is used in facilities using third party billing functionality to generate claims. This field is used for selecting an claim or service line note qualifier type that will override the type set for the billable service being overridden in the 'Note Qualifier' field on the Billable Services screen. The selection made may or may not differ from the selection set in the 'Note Qualifier' field on the Billable Services screen, for example in the case of a user wanting to only override a service's 'Claim/Service Line Note' text. The value selected in this field is exported to the NTE01 data element (Note Reference Code) of the NTE segment (Claim Note and/or Service Line Note) in either Loop 2300 or Loop 2400.
Note Text
This field is used in facilities using third party billing functionality to generate claims. This field is used for entering alternate claim or service line note text that will override the text entered for the billable service being overridden in the 'Claim/Service Line Note' field on the Billable Services screen. The text entered may or may not differ from the text entered in the 'Claim/Service Line Note' field on the Billable Services screen, for example in the case of a user wanting to only override a service's 'Note Qualifier' ('Note Type Qualifier'). The text entered in this field is exported to the NTE02 data element (Description) of the NTE segment (Claim Note and/or Service Line Note) in either Loop 2300 or Loop 2400.
Payer
This column displays the Payer/Rate Group associated with both the 'Billing Episode' selection made on this screen as well as the associated Billable Service being overridden, assuming that service has been defined on the Billable Services screen.
Episode Starting
This column displays the 'Effective Date' of the billing episode selected on this screen, as entered on the Billing Episodes screen.
Episode Ending
This column displays the 'Expiration Date' of the billing episode selected on this screen, as entered on the Billing Episodes screen.
Billable Service
This column displays the 'Billable Service' (category/primary/header type) to be overridden as selected on this screen in the 'Billable Service' field, which corresponds to the 'Billable Service' field on the Billable Services screen.
Service Type
This column displays the 'Service Type' to be overridden as selected on this screen in the 'Billable Service' field, which corresponds to the 'Service Type' field on the Billable Services screen.
Charge Option
When applicable, this column displays the 'Charge Option' selected which may or may not differ from the 'Charge Option' selected on the Billable Services screen, depending on the user's objective for entering the override record and the type of Billable Service being overridden.
Patient Rate
This column displays the US dollar amount the patient's Patient balance will be charged for the 'Billable Service' selected.
Payer Rate
This column displays the US dollar amount the patient's Third Party balance will be charged for the 'Billable Service' selected.
Note Type Qualifier
When applicable, this column displays the selection made in the 'Note Type Qualifier' field, which may or may not differ from the 'Note Qualifier' selection of the service being overridden, depending on the user's objective for entering the override record.
Note Text
When applicable, this column displays the note text entered in the 'Note Text' field, which may or may not differ from the 'Claim/Service Line Note' text of the service being overridden, depending on the user's objective for entering the override record.
We Recommend Limiting the Use of Billable Service Override Records As Much as Possible
The reason why is that managing and maintaining proper override records can be tedious and creates more opportunities for data entry mistakes, which can lead to erroneous or missing charges, and subsequently erroneous or missing claims in facilities using third party billing functionality. Additionally, often the entry of override records is completely unnecessary, and would be more optimally handled by creating additional Payer/Rate Groups and Billable Services. Payer/Rate Group and Billable Service functionality provide a much more efficient way of handling, for example, Rate changes. Billable Service Override records, while useful to accommodate unusual patient-specific scenarios, add an additional layer of complexity to Methasoft's accounting and third party billing functionality.
The Basic Dosing Charge Information Screen Automatically Creates Billable Service Override Records If 'Override...' Data is Entered
Many facilities will never need to use the Billable Service Overrides screen. However most facilities will use the Basic Dosing Charge Information screen for Self Pay-Only Rate Groups, and/or other 'Basic' Validation Level Payer/Rate Groups for a variety of reasons. Thus it's worth noting that if either of the 'Override...' checkboxes are selected on the Basic Dosing Charge Information screen and 'Override...' data is entered, behind the scenes, Methasoft automatically creates Billable Service Override records for the retrieved patient while simultaneously creating the patient's Billing Episode. Administrators and/or Accounting/Billing personnel should keep this in mind when setting up Security access to screens in their facility, because if a user accesses the Billing Episodes and/or Billable Service Overrides screen in a facility that only ever uses the Basic Dosing Charge Information screen, that user can inadvertently cause problems by changing the way a patient is charged. In many facilities, primarily Self Pay-Only facilities, we recommend that access to the Billing Episodes and/or Billable Service Overrides screen should be denied, because there should be no need to access them - the Basic Dosing Charge Information screen will handle all needed changes for them, making the process of setting up a patient to be charged much clearer and less confusing.
Currently Override Records are Limited to Absent Charges, Managed Dosing and Unmanaged Dosing Billable Service Types
Though other types of 'Billable Service': 'Service Type' combinations are available on the Billable Services screen, override functionality on this screen is currently only available for managed and unmanaged Dosing services, as well as Absent Charge services. Additional service types may become available in future versions of Methasoft.
Unmanaged: Dosing Periodic Billable Service Types can be Overridden to Any of the 4 Applicable Charge Options (Per Week, Per Month, Semi-Monthly, 4x/Month (Mon))
Though the most common use for entering a billable service override record is to charge a patient one or more different rate(s), or to charge a patient on a different day of the week or month, this screen can be used, for example, to override an Unmanaged: Dosing Periodic 'Per Week' billable service to 'Semi-Monthly' or '4x/Month (Mon)'. Just beware of the potential confusion that could result if users are not fully educated on override records and how they work, and are focusing only on Billable Service configurations and then wondering why a patient is not being charged accordingly due to the existence of an override record.
When Overriding Only One Type of Rate, Be Sure to Still Include a Rate Amount for the Other Type of Rate Not Being Overridden
One of the most common uses of this screen is to charge a patient a different Patient Rate and/or Payer Rate than the rate(s) defined for the associated billable service on the Billable Services screen. A common mistake we have observed is that when entering an override record, the user will want only one of these two rates to be different, and will not address the other type of rate on the Billable Services Override screen. Since both fields are required fields in order to save the override record, and since users may not have access to the Billable Services screen, we've seen users enter $0 in the rate field they don't wish to override, assuming that the system will use the default service rate defined on the Billable Services screen. But this will not work, unless the default rate defined in Billable Services happens to be $0. Thus it always a best practice to know both of the rates for the service being overridden, so that if only one rate is changed on the Billable Service Overrides screen, the other default rate is also appropriately entered in the field for the rate not being overridden.
When Overriding the Note Type Qualifier and/or Note Text
Very much related to the Consideration above this one regarding rates, it is a best practice to always know the 'Claim/Service Line Note' text and 'Note Qualifier' selection defined on the Billable Services screen if a user wishes to override the data in one of these fields but not the other on the Billable Service Overrides screen. Even if only one field is being overridden, the other related field must contain the correct data, or inaccurate note data might end up being exported for claims on EDI export billing files.
After Deleting a Billing Episode for a Patient, Delete any Associated Billable Service Override Records as Well
Though deleting a patient's Billing Episode should be rare, when a user deletes a patient's billing episode on the Billing Episodes screen, Methasoft does not currently delete any associated Billable Service Override records. Though functionally this will not cause any problems, when applicable, to avoid potential unnecessary confusion, it is a best practice to delete any associated override records before or after deleting a patient's billing episode.
Dynamic Enable / Disable, Cascading (Filtered) Dropdown Selections, and Required Field Functionality
This screen includes functionality that will automatically enable or disable fields, filter subsequent dropdown combo field selection lists, and/or require fields dynamically depending on the selections made in other related fields. For example, if no value is selected in a Secondary ID Code Type field, then the Secondary ID Code field will be disabled. But once a value is selected in the Secondary ID Code Type field, not only does the Secondary ID Code field become enabled, it also becomes required. An example of Cascading (Filtered) Dropdown functionality is when a value selected in one combo dropdown field determines which dropdown values are available for selection in another dropdown field by filtering out invalid selections. This functionality exists to minimize erroneous data entry, and particularly the generation / export of invalid EDI files such as the 837P, which will be rejected by either a clearinghouse and/or payer. This functionality is in addition to, and when applicable will override, initial required field functionality which operates when a New record is being entered, no data is entered in any field, and the Save button is pressed.
Basic Dosing Charge Information
Claims Generator
Claims Generator - Edit Service Lines - Billing Service Line Management
Billing Export
Batch Payments
Understanding the 837 Professional (837P) Export File Format
Loop 2300 (Claim data)
Loop 2400 (Service Line data)
Troubleshooting EDI File and Claim Rejections/Denials
Aging Claims
Batch Payments
Billable Services
Billable Units Summary by Payer
Billing Episodes Expiring
Claims by Payer
Claims Summary
Intakes and Discharges by Modality
Missing Charges
No Show Preview Today by Counselor
No Show Summary by Patient
Outstanding Claims
Patient and Payer Charges
Patient Insurance Eligibility
Patient List by Billing Episode
Patient List by Modality/Payer
Patient List by Payer
Patient List History by Payer
Patient Medication Record Breakdown by Payer
Patient Medication Record for Billing
Payment Information Patient Charges Dosing
Service Checks
Service Lines by Claim
Service Lines by Service