![]()
![]()
(Topic Last Updated On: 04/06/2015)
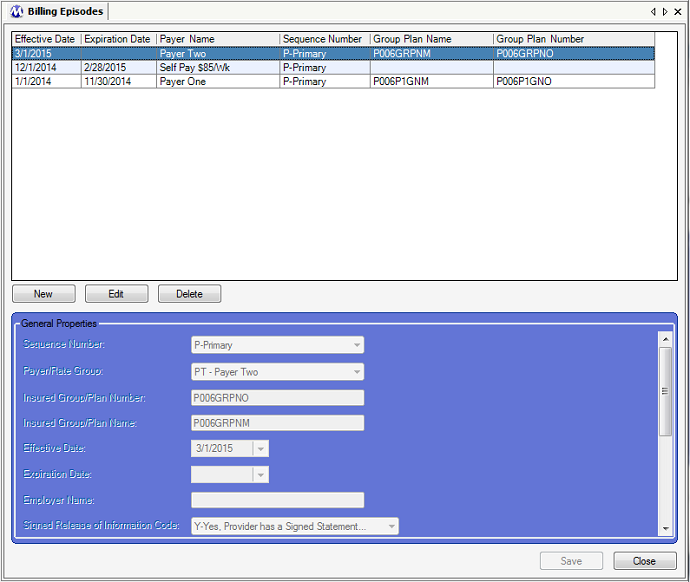
The Billing Episodes window is accessed from the Accounting menu, and replaces the Patient Insurance Episodes screen found in versions of Methasoft prior to version 6, as well as the old 'Current Insurance Episode' section of the Payment Information screen. When a patient is retrieved on this screen, the patient's entire Billing Episode history is presented, including the patient's current/effective episode as highlighted in the screen shot below. A Billing Episode is associated with a Payer/Rate Group, which allows Methasoft to know how to charge the patient for services rendered in facilities using both Self Pay and/or Third Party Billing functionality, via the defined Billable Services for each Payer/Rate Group. A patient will not be charged for any billable service unless the patient has a saved current/effective Billing Episode which is associated with a Payer/Rate Group that is associated with one or more current/effective Billable Services. Thus without a Billing Episode, a patient at the Dosing window will not be able to be dosed in Methasoft unless the patient has a current/effective Billing Episode associated with a Payer/Rate Group that is associated with a current/effective Managed Dosing or Unmanaged Periodic Dosing Billable Service. Billing Episode effective date ranges cannot overlap, and can be entered either directly on this screen or on the Basic Dosing Charge Information for Dosing services associated with 'Basic' Validation Level Payer/Rate Groups (for Self Pay Rate Groups). This screen includes conditional field requirement functionality based on the Validation Level (Basic or Advanced) of the selected Payer/Rate group. Only 2 fields are required if a Basic Payer/Rate Group is selected, whereas additional fields are required for Advanced Payer/Rate Groups based on the assumption that these Payer/Rate Groups are being used for integrated Third Party Billing functionality including Claims generation and/or EDI Billing Export file generation.
Sequence Number
For facilities using Third Party Billing functionality, this field is related to Coordination of Benefits (COB) functionality currently being developed. This field is used for selecting the sequence number of the Payer being selected. If a Billing Episode is associated with more than one Payer, then the selection made in this field for each episode record will ultimately drive the sequence in which submitted claims are adjudicated and submitted to each Payer involved. This field is a required field under any circumstance, and 'P - Primary' is selected by default in this field because it is generally the only selection used. 'S - Secondary' is available for selection in this field for currently limited COB functionality used in some facilities. 'P - Primary' should always remain selected for Self Pay Basic Validation Level Payer/Rate Group episodes if they are entered on this screen. For 837P EDI billing export files, the value selected in this field is exported to data element SBR01 (Payer Responsibility Sequence Number Code) of the SBR segment (Subscriber Information) of Loop 2000B (Subscriber Hierarchical Level).
Payer/Rate Group
This field is always required and is used for selecting the Payer/Rate Group to be associated with the Billing Episode being entered. This field is populated by all Payer/Rate Groups entered on the Payer/Rate Groups screen, and is the primary data used by Methasoft to properly charge a patient for billable services rendered. The only way Methasoft will allow you to enter Billing Episodes with overlapping effective date ranges is if the Payer/Rate Group selected in this field along with the value selected for it in the 'Sequence Number' field above vary from those of the episode being overlapped.
Insured Group/Plan Number
This field is optional, but is sometimes used in facilities using Methasoft's Claim generation and/or EDI Billing Export functionality if required by a clearinghouse and/or Payer. Data entered in this field is exported to data element SBR03 (Reference ID) of the SBR segment (Subscriber Information) of Loop 2000B (Subscriber Hierarchical Level).
Insured Group/Plan Name
This field is optional, but is sometimes used in facilities using Methasoft's Claim generation and/or EDI Billing Export functionality if required by a clearinghouse and/or Payer. Data entered in this field is exported to data element SBR04 (Name) of the SBR segment (Subscriber Information) of Loop 2000B (Subscriber Hierarchical Level).
Effective Date
This field is always required and is used for selecting the first date on which the entered episode is effective, resulting in Methasoft charging a patient accordingly due to the episode's association with a Payer/Rate Group and the Payer/Rate Group's Billable Service(s). This date can be back-dated to accommodate situations where either an erroneous date was selected, or for any scenario that results in a patient being charged erroneously. The only way Methasoft will allow you to enter Billing Episodes with overlapping effective date ranges is if the Payer/Rate Group selected in this field along with the value selected for it in the 'Sequence Number' field above vary from those of the episode being overlapped.
Expiration Date
This field is not required and is used for selecting the last date on which the entered episode is effective, resulting in Methasoft charging a patient accordingly due to the episode's association with a Payer/Rate Group and the Payer/Rate Group's Billable Service(s). This date is no required so that a patient's Billing Episode can remain open-ended and never expire. This date can be back-dated to accommodate situations where either an erroneous date was selected, or for any scenario that results in a patient being charged erroneously. The only way Methasoft will allow you to enter Billing Episodes with overlapping effective date ranges is if the Payer/Rate Group selected in this field along with the value selected for it in the 'Sequence Number' field above vary from those of the episode being overlapped.
Employer Name
This field is optional and purely used for informational purposes within your facility. The data entered this field is not exported to EDI Billing Export files.
Signed Release of Information Code
This field is required for 'Advanced' Validation Level Payer/Rate Groups, and is used for selecting whether or not a patient has signed a release of information consent form maintained by the rendering provider allowing for the release of all medical data necessary for the adjudication of a claim, or if the patient has not signed such a release but has expressed informed consent for the release of such medical data in states where a signed release is not required by law, and assuming no prohibition of such by federal law. For the 5010 EDI format standard only one of 2 acceptable values can be selected in this field, 'I - Informed Consent to Release Medical Info...' or 'Y - Yes, (service) provider has a signed statement'. Most commonly the latter value is selected in this field, but only after a signed consent for the release of medical info has been obtained. The value selected in this field is exported to data element CLM09 (Release of Information Code) of the CLM segment (Claim Information) of Loop 2300 (Claim Information).
Patient Signature Source Code
This field is optional and rarely used. If used, it used to indicate that a patient's signature to release medical data for claim adjudication was 'generated' (signed) by the service provider on the patient's behalf to accommodate unusual scenarios, and only if allowed by state and federal law. The only acceptable value for the 5010 EDI format standard is 'P - Generated by (service) provider'. If a value is selected in this field, the value selected is exported to data element CLM10 (Patient Signature Source Code) of the CLM segment (Claim Information) of Loop 2300 (Claim Information).
Subscriber Entity Type
This field currently only exists for potential future functionality. Currently the value '1 - Person' is selected by default in this field and should be left alone for any Billing Episode entered, because currently it is impossible in Methasoft for the Subscriber to be anything other than a Patient (see 'Considerations' below). The value selected in this field is exported to data element NM102 (Entity Type Qualifier) of the NM1 segment (Subscriber Name) of Loop 2010BA (Subscriber Name).
Subscriber ID Code Type
This field required if an 'Advanced' Validation Level Payer/Rate Groups is selected, and is used for selecting the Primary Subscriber ID Type for the retrieved patient's Billing Episode. The most common value selected in this field is 'MI - Member ID Number'. The value selected in this field is exported to data element NM108 (ID Code Qualifier) of the NM1 segment (Subscriber Name) of Loop 2010BA (Subscriber Name).
Subscriber ID Code
This field required if an 'Advanced' Validation Level Payer/Rate Groups is selected, and is used for selecting the Primary Subscriber ID for the retrieved patient's Billing Episode, as assigned by a Clearinghouse and/or Payer. The value entered in this field is exported to data element NM109 (ID Code) of the NM1 segment (Subscriber Name) of Loop 2010BA (Subscriber Name).
Subscriber Secondary ID Code Type
This field is optional and is only used when a Clearinghouse and/or Payer requires that Secondary Identification data be submitted for claim adjudication. When used, this field is used to select the type of Secondary ID being submitted. The EDI 5010 format standard allows only the 'SY - Social Security Number' type to be submitted. The value selected in this field is exported to the data element REF01 (Reference ID Qualifier) of the REF segment (Subscriber Secondary ID) of Loop 2010BA (Subscriber Name).
Subscriber Secondary ID Code
This field is optional and is only used when a Clearinghouse and/or Payer requires that Secondary Identification data be submitted for claim adjudication. When used, this field is used to the retrieved patient's Secondary ID being submitted. The EDI 5010 format standard allows only the patient's Social Security Number to be submitted. The SSN entered in this field is exported to the data element REF02 (Reference ID) of the REF segment (Subscriber Secondary ID) of Loop 2010BA (Subscriber Name).
Benefits Assignment Indicator
This field is required for 'Advanced' Validation Level Payer/Rate Groups, and is used for selecting whether or not the insured patient has authorized the Payer to remit payment directly to the service provider. The most common value selected in this field is 'Y - Yes', once the insured patient has made this authorization. The nature of this authorization, verbal or documented, should be determined by your facility in accordance with state and federal regulations. The value selected in this field is exported to data element CLM08 (Benefit Assignment Certification Indicator Response Code) of the CLM segment (Claim Information) of Loop 2300 (Claim Information).
Referring Provider
This field is optional and is populated by all Referring Providers entered on the Referring Providers screen. This field is used for associating a patient's Billing Episode with the Referring Provider selected. If a Referring Provider is selected, then NM1 (Referring Provider Name) and when applicable, REF (Referring Provider Secondary Identification) segment data will be exported to Loop 2310A (Referring Provider Name - Claim Loop) on 837P EDI billing export files for facilities required to submit this data to third party Payers. Generally this field is left blank. See the 'Considerations' section below for more detailed information on this field.
Effective Date
This column displays the selected 'Effective Date' for each billing episode, which is the first date on which Methasoft will charge a patient accordingly.
Expiration Date
This column displays the selected 'Expiration Date' for each billing episode, which is the last date on which Methasoft will charge a patient accordingly.
Payer Name
This column displays the 'Payer/Rate Group' selected for each billing episode, which associates the retrieved patient with the Billable Service(s) the patient will be charged for.
Group Plan Name
This column displays the 'Insured Group/Plan Name' entered for each billing episode, which may or may not be required by a Clearinghouse and/or Payer.
Group Plan Number
This column displays the 'Insured Group/Plan Number' entered for each billing episode, which may or may not be required by a Clearinghouse and/or Payer.
In Methasoft, the Subscriber is the Patient
The 837P EDI format supports a 3rd Hierarchical Level (HL3) which differentiates a Subscriber (HL2) from a Patient (HL3). However, for Methasoft users we've never encountered the need to implement this distinction, despite that the underlying architecture is in place to do so. Thus, in Methasoft, the Subscriber is always the Patient.
Using the Basic Dosing Charge Information Screen Instead of Entering Billing Episodes
Especially for Self Pay-Only facilities, using the Basic Dosing Charge Information screen is generally more efficient and intuitive to users than using the Billing Episodes screen when setting up how patients will be charged in Methasoft, and thus is recommended. Some facilities however have a mix of both Self Pay and Insured (Third Party) patients, in which case it is up to your facility to determine if it is advantageous to use both of these screens, in lieu of solely using the Billing Episodes screen. See the Basic Dosing Charge Information topic for more details, because saving a patient's Basic Dosing Charge Information automatically creates or updates Billing Episode records behind the scenes.
Payer/Rate Group Validation Level - 'Basic' vs. 'Advanced' - Different Required Fields
There is a core set of required fields regardless of the 'Payer/Rate Group' selected on this screen. However very few fields are required for 'Basic' Validation Level Rate Groups (used for Self Pay patients) compared the number of fields required for 'Advanced' Validation Level Payers (used for Insured / Third Party patients). This is because for Insured / Third Party patients, it is assumed that Claims and/or EDI Billing Export files will be generated, and in order for these generated items to be valid, the data required on this screen for 'Advanced' Payers is necessary.
Editing or Deleting Billing Episode
Methasoft attempts to cover as many scenarios as possible to prevent users from creating bad data, or losing data, inadvertently by editing or deleting a Billing Episode that is currently in use or has been previously associated with generated charges and/or claims. However users should use caution and really think through the change being made, particularly in regards to which fields are being affected (of course Deleting an episode affects the entire episode record, and thus all fields). For example, editing the 'Employer Name' of a Billing Episode is unlikely to cause any real harm. Whereas, for example, editing the Effective date range of a Billing Episode could potentially cause a wide range of problems which cannot be quickly fixed. If you are uncertain about the ramifications of editing or deleting a Billing Episode, please confirm what you are about to do internally with someone at your facility, or contact Methasoft Customer Support prior to editing or deleting the Billable Service.
Editing or Deleting Billing Episodes for Third Party Billing - Potential Timing/Workflow Issues Related to Claim Generation/Billing Export
Related to the Consideration above this one, when editing a Billing Episode for which claims are being exported, it is important to consider the timing of the edit. For example, some data entered on this screen is retrieved at the time of exporting generated Claims. Thus, if Claims have already been exported but not yet submitted to a Payer, it is generally a good rule of thumb to edit the Billing Episode data then re-export the unsubmitted Claims. All staff responsible for billing activities within a facility should make sure they understand the billing workflow within their facility, and communicate changes that are being made in Methasoft accordingly, in order to minimize billing export file rejection. Similar examples apply to the timing of claim generation, along with the timing of export file generation and/or submission. And all of these principles apply when deleting a Billing Episode, even more than when editing an episode.
Billable Service Override Records are Associated with Billing Episodes
When Billable Service Override Records are entered in Methasoft, each is associated with specific Billing Episode. Thus it's important for users to be aware of this when editing or deleting a Billing Episode in order to also delete any associated Billable Service Override records. It's also important when troubleshooting erroneous charges found. In such cases, often the Payer/Rate Group, Billable Service, and Billing Episode data is correct, but there's an overlooked Billable Service Override record that is overriding the associated Billable Service and causing the patient to be charged differently than expected.
Overlapping Billing Episodes
The only way Methasoft will allow you to enter Billing Episodes with overlapping effective date ranges is if the Payer/Rate Group selected in this field along with the value selected for it in the 'Sequence Number' field above vary from those of the episode being overlapped. Thus if your facility is not using Methasoft's COB functionality, Methasoft will prevent you from entering Billing Episodes with overlapping effective date ranges.
Dropdown Selection Fields - (4010) and (5010) Value Indicators
In numerous dropdown selection fields used on various Billing-related screens, you will notice '(5010)', '(4010)', or nothing following each value. These indicators are there to allow Methasoft to continue to support customers submitting 4010 EDI files until the transition from 4010 to 5010 is fully complete, at which time deprecation of 4010 functionality is expected. If '(5010)' appears following a value, this means that the value is only valid for 5010 EDI file submissions. If '(4010)' appears following a value, this means that the value is only valid for 4010 EDI file submissions. If nothing appears following a value, this means that the value can be legitimately used for both 4010 or 5010 EDI file submissions (i.e., these values were carried over from 4010 to 5010).
Referring Provider Data is Currently Only Exported at the Claim Level (Loop 2310A)
In a facility exporting Referring Provider data, it is important to note that a Referring Provider can currently only be associated with a Patient via the Billing Episodes screen, which is not Service-specific. This means that if a Referring Provider is selected in this field and associated with a patient's Billing Episode, the selecting Referring Provider's data will only be exported at the Claim level using Loop 2310A of the 837P EDI file. This means the Referring Provider's data will apply to all Service Lines of a patient's Claim, regardless of the Billable Service Type(s) rendered.
Basic Dosing Charge Information
Claims Generator - Edit Service Lines - Billing Service Line Management
Understanding the 837 Professional (837P) Export File Format
Loop 2000B (Subscriber Hierarchical Level data)
Loop 2010BA (Subscriber Name data)
Loop 2300 (Claim Information data)
Troubleshooting EDI File and Claim Rejections/Denials
Aging Claims
Batch Payments
Billable Services
Billable Units Summary by Payer
Billing Episodes Expiring
Case Notes Billable Units by Payer
Case Notes Billable Units Summary by Payer
Caseload Summary by Payer
Claims by Payer
Claims Summary
Intakes and Discharges by Modality
Missing Charges
No Show Preview Today by Counselor
Outstanding Claims
Patient and Payer Charges
Patient Insurance Eligibility
Patient List by Billing Episode
Patient List by Modality/Payer
Patient List by Payer
Patient List for Billing by Counseling Category
Patient List History by Payer
Patient Medication Record Breakdown by Payer
Patient Medication Record for Billing
Prior Authorizations
Service Checks
Service Lines by Claim
Service Lines by Service
Automatically insert default Payment Information on new patients
Default payer when assigned automatically