![]()
![]()
(Topic Last Updated On: 09/14/2015)
The Billing Eligibility menu item on the Accounting menu launches the Billing Eligibility screen, which is used by facilities using Methasoft's third party billing functionality to view the results of 270 EDI Health Plan Benefit Coverage requests set to third party Payers. These results are populated based on the 271 EDI message received from the Payer and/or Clearinghouse. The Search criteria fields allow users to filter the results by Sent Date, Payer, Status, Patient ID, and/or Requested By (the Methasoft user who initiated the Eligibility Check). The Status column is color-coded to clearly identify which patients have Active coverage, Inactive coverage, requests that have been Sent but not yet responded to, and requests which generated an Error at some point within the 270 inquiry/271 response cycle. The Details button can be pressed for a selected Eligibility Check to show a window with detailed information received on the 271 EDI response. This screen is integrated with the Messages panel on the left side of the Methasoft user interface, so that when Billing Eligibility Checks Sent or Received links are pressed, this screen opens and displays the corresponding messages on the grid. The Create/Send Batch button is used to launch a Select Patient window, where users can filter the list of available patients to include for sending batch 270 EDI transmissions.
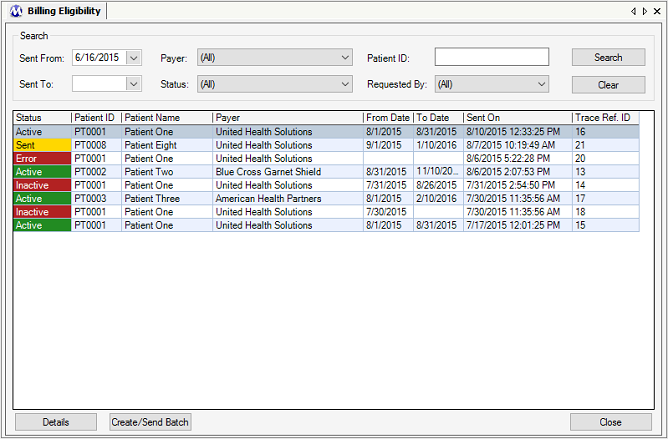
Sent From
This field is used to filter the responses shown on the grid by selecting the date on or after an eligibility check was sent. When this screen is opened, this field is auto-populated with a date 90 days prior to the current date.
Sent To
This field is used to filter the responses shown on the grid by selecting the date on or before an eligibility check was sent.
Payer
This field is used to filter the responses shown on the grid by displaying only eligibility checks for the Primary Payer/Rate Group associated with the patient's current / effective Billing Episode at the time an eligibility check was sent. The Primary Payer/Rate Group shown may or may not match the Primary Payer/Rate Group associated with the patient's current / effective Billing Episode, because this screen always displays the Primary Payer/Rate Group at the time at which the eligibility check was sent, after which a patient's Billing Episode could end and a new one be created with a different Primary Payer/Rate Group.
Status
This field is used to filter the responses shown on the grid by displaying only eligibility checks of the selected Status.
Patient ID
This field is used to filter the responses shown on the grid by displaying only eligibility checks sent for the entered Patient ID.
Requested By
This filter is used to filter the responses shown on the grid by displaying only eligibility checks sent by the selected Methasoft User ID.
Status
This column is color-coded and displays the status of each eligibility check based on the 271 EDI response message received. 'Sent' indicates that the outgoing 270 message was sent, but has not yet been responded to. 'Active' indicates that the returned 271 message indicated the patient's insurance coverage is active for the date range provided. 'Inactive' indicates that the returned 271 message indicated the patient's insurance coverage is inactive for the date range provided. 'Error' indicates that a 270 message was generated and sent, but that somewhere along the path to the clearinghouse and/or third party payer through the returned 271 message, an error occurred while processing either the 270 or 271 message.
Patient ID
This column displays the Patient ID of the patient for each eligibility check response.
Patient Name
This column displays the First and Last Name of the patient for each eligibility check response.
Payer
This column displays the Primary Payer/Rate Group to which each eligibility check was sent, based on each patient's current / effective Billing Episode at the time each eligibility check was sent.
From Date
This column displays the Effective Date of each patient's Health Plan Benefit Coverage as returned by the Payer/Rate Group on the 271 EDI response message.
To Date
This column displays the Expiration Date of each patient's Health Plan Benefit Coverage as returned by the Payer/Rate Group on the 271 EDI response message.
Sent On
This column displays the date and time on which each 270 EDI eligibility check message was sent.
Trace Ref. ID
This column displays the unique Trace Reference Number generated by Methasoft when each 270 EDI message was generated. This value is exported in a TRN segment of the outgoing 270 EDI check message, and is returned in a TRN segment of the incoming 271 EDI response message.
Search
Pressing this button will populate the grid with eligibility check records / responses based on the Search criteria field selections made.
Clear
Pressing this button will clear the Search criteria fields and return the screen to its initial state, displaying all eligibility checks / responses sent over the past 90 days.
Details
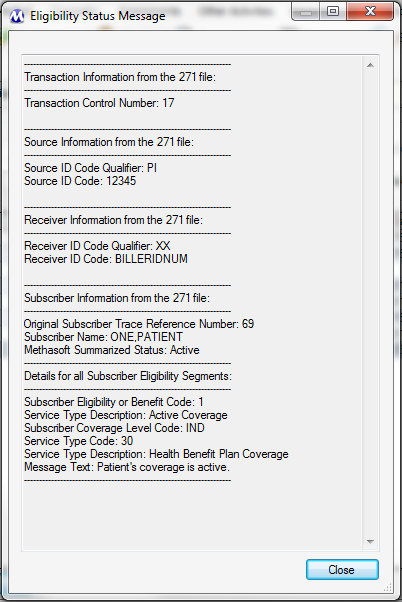
Pressing this button or double-clicking on a grid row will open the Eligibility Status Message window for the selected check / response as shown in the screen shot below. This window displays additional detailed information for each 271 EDI response received.
Create/Send Batch
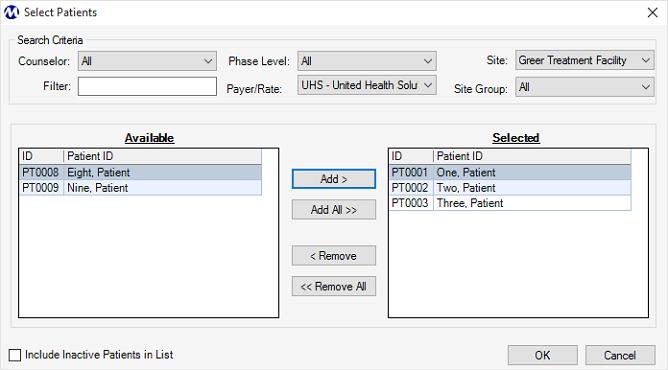
Pressing this button opens the Select Patient window shown below, which allows users to filter the list of Available patients then add them to the list of Selected patients for whom a batch of eligibility checks will be sent when the Ok button is pressed.
Close
Pressing this button closes the Billing Eligibility screen.
Eligibility Checks Require Patients to Have a Current / Effective Billing Episode Associated with a Third Party Payer/Rate Group
Outgoing 270 EDI eligibility check messages can only be sent to a third party Payer or clearinghouse, who sends it to a third party Payer. This requires that a patient for whom an eligibility check is being performed has a current / effective Billing Episode containing the necessary data (e.g., Subscriber / Member ID) for a valid 270 EDI message to be generated. Generally such Payer/Rate Groups are set up in Methasoft with an 'Advanced' Validation Level, which requires more data entry on Billing Episodes and other screens than 'Basic' Validation Level Payer/Rate Groups, to ensure that valid 837P, 835, and/or 270/271 EDI messages are valid.
Payer/Rate Groups to Whom Eligibility Checks are Submitted Must be Associated with a Properly Configured Receiver Format Record
On the Payer/Rate Groups screen, the 'Receiver Format' field is used to associate a third party Payer/Rate Group with a Receiver Format record. This is necessary so that ISA header segment data is valid for outgoing 270 EDI messages, as well as for defining the delimiters that will be used to separate segments, data elements, and components (sub-elements).
Associated Receiver Format Records Must Be Properly Configured in Order for Outgoing 270 EDI Messages to Receive a Valid 271 EDI Response
Before your facility begins sending Eligibility Check (270 EDI) messages, it's important that all information for one or more associated Receiver Format records is properly configured. Missing or invalid ISA and/or Delimiter data will result in invalid 270 EDI messages, which will be rejected by a clearinghouse and/or third party Payer.
Additional Configuration Might be Necessary for Your Facility to Submit Outgoing 270 EDI Messages to Receive Valid 271 EDI Responses
Before your facility begins sending Eligibility Check (270 EDI) messages, various system configuration settings and/or Preferences (System-Preferences) must be set properly. Depending on your facilities needs, some configuration settings might require intervention by Methasoft Training, Support, or Technical staff. Contact Methasoft Customer Support at (877) 538 - 5767 for help.