![]()
![]()
Chapter Four: Accounting Menu
(Topic Last Updated On: 03/12/2015)
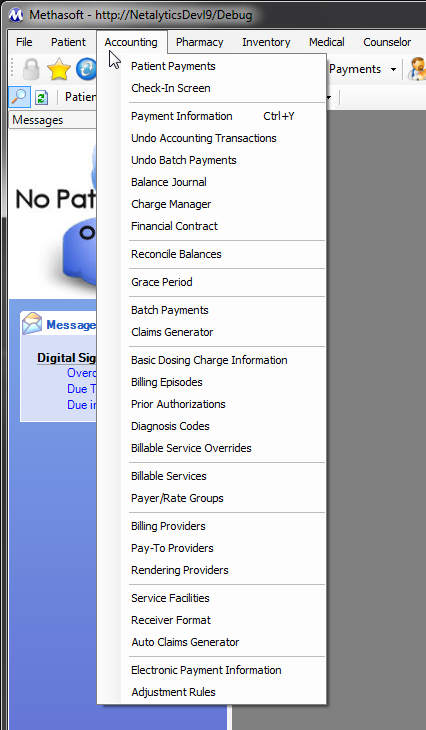
The Accounting menu displayed in the screen shot above is accessed by clicking on the Accounting main menu item. This menu contains menu items that launch screens or windows which provide system functionality generally used by Accounting, Billing, Front Desk, and/or Reception personnel.
The Patient Payments screen is used to review Balance information, record Payments, add Additional Debits and Credits, check patients in, read Flag Messages and direct patients to facility areas and staff accordingly, send Quick Dosing Flag messages, and provides additional buttons in the toolbar at the top for accessing additional functionality.
The Check-In Screen is a highly stripped-down version of Patient Payments, allowing for non-Accounting staff to check patients in for Dosing, often used, for example on the weekends. Limited, additional functionality is also available on the Check-In Screen.
The Payment Information screen is used to store miscellaneous payment and/or accounting information for each patient. The Payment Information screen changed significantly from Methasoft Version 5 to Version 6, in light of the overhaul of Accounting and Billing functionality implemented for Version 6. The Payment Information screen also provides patient-specific 'Override Balance Locking' functionality allowing facilities to make exceptions for individual patients in regards to the Maximum Patient Balance amount a patient can carry in order to be dosed.
The Undo Accounting Transactions window is used for Undoing any Patient or 3rd-Party Balance accounting transaction for the retrieved patient, including 'Reason' and 'Comments' fields for noting why the selected transaction is being undone.
The Undo Batch Payments screen is used for Undoing a Batch Payment applied then saved on the Batch Payments screen, including 'Comments' fields for noting why a Batch Payment is being undone. This screen is very helpful in facilities using Batch Payment functionality as it allows users to undo an entire Batch Payment in one transaction, as opposed to having to undo Batch Payments individually applied for each patient.
The Balance Journal screen displays details for each accounting transaction recorded for a patient for any Balance Type, including voided transactions that were undone.
The Charge Manager screen allows users to view, generate, regenerate and/or delete charges in Methasoft based on the Billable Service Criteria entered at the top of the screen. Generally this screen is used to correct erroneous charges generated by Methasoft automatically based on incorrect Billing Episode, Billable Service, and/or Billable Service Override data. It's also used to back-generate charges, most commonly in light of Billing Episode and/or Billable Service Effective date range changes. This screen is very useful for correctly large batches of erroneous charges in one transaction.
The Financial Contract screen is used for scheduling patient repayment plans for patients who have accounts with overdue balances. Financial Contracts can be printed at the time a contract is saved, and the resulting report printed lists all scheduled payment due dates and amounts, and provides a signature line for the patient to sign in order to make it a binding contract.
The Reconcile Balances window is used to accommodate unusual circumstances, which lead to one or more Patient balances of any type in need of being adjusted to a different Balance amount, either negative or positive. Security access to this window is often limited to Administrative staff only.
The Grace Period window is used in facilities that use Methasoft's Grace Period functionality, for automatically scheduling Administrative Detoxes and/or Detox reversals based on the retrieved patient's Overdue Balance amount and how long the patient's balance has been overdue. This window allows facilities to override global Grace Period settings defined in Methasoft Preferences for individual patients to accommodate patient-specific conditions.
The Batch Payments screen is used for efficiently viewing, applying and/or adjusting large batch Third Party payments towards individual Service Lines and/or Claims in facilities using Methasoft's Billing functionality. 835 functionality has been integrated with this screen allowing new 835 files to be loaded and posted toward patient accounts.
The Claims Generator screen is used in facilities generating Claims and Service Lines for Billable Services rendered to patients, generally for either generating and submitting an electronic billing claim (Billing Export EDI file), or for using this data to submit claims manually and/or through another third party system. This screen allows Billing personnel to easily generate Claims and Service Lines based on the Service Criteria entered at the top of the screen. The Edit Service Lines button opens the Billing Line Service Management window, where the individual Service Lines of a Claim can be reviewed, and in some cases edited or deleted.
The Basic Dosing Charge Information screen was implemented for Methasoft Version 6, primarily as a replacement for the Payment Information screen for facilities with Self-Pay patients, allowing such facilities to efficiently set up how a retrieved Self-Pay patient will be charged for Dosing Billable Services, without requiring the use of the Billing Episodes and/or Billable Service Overrides screen(s). Only Payer/Rate Groups set up with a 'Basic' Validation Level on the Payer/Rate Groups screen and associated Dosing Billable Service data will appear available for selection on this screen.
The Billing Episodes screen is used for entering Billing Episodes for insured patients for Third Party Billing functionality. A patient's Billing Episode have an Effective date range and is associated with a Payer/Rate Group, which determines how Methasoft will charge the patient for rendered Billable Services, as well as specific Billing Export EDI file values to be exported. Coordination of Benefits (COB) functionality is currently being developed to support billing multiple Payers for patients with more than one insurer. Billing Episodes can also be directly associated with Billable Service Override records on the Billable Service Overrides screen, allowing individual patients to be charged differently than as defined by the default Billable Service(s) involved.
The Prior Authorizations screen is used for entering Prior Authorization numbers and Effective date ranges for one or more Billable Services as assigned to each patient by one or more Payers. Prior Authorization numbers are then exported at the Claim and/or Service Line level as needed, on Billing Export EDI files. Prior Authorizations can be entered for an Authorization Type that covers multiple Service Types, or for a specific Service Type.
The Diagnosis Codes screen is used when necessary to override the ICD-9 or ICD-10 Diagnosis Code set globally for each Billable Service on the Billable Services screen. Up to 4 ICD-9 or ICD-10 Diagnosis Codes can be entered for a retrieved patient and associated with the specific Billable Service Type to be overridden. Diagnosis Codes entered on this screen are then exported to Billing Export EDI files accordingly for specific patients.
The Billable Service Overrides screen should be used minimally, but is used to accommodate unusual scenarios for an individual patient by overriding the way a patient is charged for one or more Billable Services. This screen is also used if a Payer requires a unique, patient-specific Claim or Service Line note text to appear on exported Billing EDI files for one or more Billable Services.
The Billable Services screen is used by every facility to configure how patients will be charged for services rendered to them. Each service configured is associated with a specific Payer/Rate Group, and this screen is used to configure Billable Services for both Self-Pay Rate Groups and Third Party Payers. Some Billable Service data is used for generating and/or exporting billing Claims and Service Lines, and the More... button provides additional service settings for each service.
The Payer/Rate Groups screen is used by every facility to configure the Self-Pay Rate Groups and Third Party Payers necessary for associating with configured Billable Services. Each facility should carefully think though the Payer/Rate Groups needed for their facility, as doing so will allow more efficient use of the Basic Dosing Charge Information, Billing Episodes, Billable Services, Billable Service Overrides, Charge Manager, Claims Generator, and/or Billing Export screens / windows as needed.
The Billing Providers screen is used in facilities using Methasoft's Third Party Billing functionality. Much of the Billing Provider data entered on this screen is exported on Billing Export EDI files. Each Billing Provider entered on this screen is associated with a Receiver Format record on the Receiver Format screen, allowing facilities to configure multiple Receiver Format records if necessary.
The Pay-to Providers screen is used in facilities using Methasoft's Third Party Billing functionality, when necessary. Generally this screen is not used because generally a facility's Pay-to Provider is the same entity as the facility's Billing Provider, in which case Pay-to Provider data is not exported on Billing Export EDI files. However, if a facility's Pay-to Provider is a different entity than the facility's Billing Provider, then this screen is used to enter Pay-to Provider data. A Pay-to Provider entered on this screen must be associated with one or more Receiver Format records in order for the Pay-to Provider's data to be properly exported on Billing Export EDI files.
The Rendering Providers screen is used to enter all Rendering Providers rendering Billable Services to patients. This screen is critical for facilities using Third Party Billing functionality to generate and/or export Claims and Service Lines. Rendering Providers are associated with Billable Services on the Billable Services screen, either specifically, or using the 'Entered By' Rendering Provider Type, in which case each Methasoft User who is a Rendering Provider must be associated with Rendering Provider records using the Billing Assoc. button on the Employee Profile screen accessible from the Administration menu. Rendering Providers are associated with Service Lines (and thus Claims), allowing Rendering Provider data to be exported at the Service Line and/or Claim level on Billing Export EDI files depending on a Clearinghouse and/or Payer's requirements.
The Service Facilities screen is used to enter all Service Facilities at which Billable Services are rendered to patients. Generally there is only one record entered on this screen, which is your facility. A Service Facility is then associated with each Billable Service on the Billable Services screen. Service Facility data is associated with generated and/or exported Service Lines and Claims.
The Receiver Format screen is used in facilities that are generating and/or exporting Service Lines and Claims for submission to Third Party Payers. Generally only one record is entered on this screen, however it allows for multiple records to be entered in facilities with unique Third Party Billing needs. Each Receiver Format record is associated with a Billing Provider and/or Pay-to Provider so that the appropriate data is exported for each when a Receiver Format record is selected on the Billing Export window. Receiver Format records also dictate numerous additional Billing Export EDI file properties depending on a facility's needs.
The Auto Claims Generator screen is used in facilities that are generating and/or exporting Service Lines and Claims for submission to Third Party Payers. This screen allows facilities to configure automatic Service Line and Claim generation for specific Billable Service Types. Methasoft Nightly Processes then generate Service Lines and Claims for configured Billable Services accordingly.
The Electronic Payment Information screen is primarily used to store Electronic Payment Method information for each patient, which generally means Debit or Credit Card information. However other Payment Method type data not associated with electronic forms of payment can also be stored on this screen, such as information for a third party who is paying a facility by check on behalf of a patient. This screen includes validation functionality designed to prevent erroneous Debit or Credit Card information to be entered.
The Adjustment Rules screen is used to create conditional rules for facilities importing 835 EDI files (ERAs) on the Batch Payments screen to apply and save third party Batch Payments towards claimed Service Lines. Adjustment Rules can be configured at the Payer or Billable Service level, and determine how Service Adjustments (CAS segments) and/or 'Remaining' Service Line amounts are automatically handled when an 835 file is imported (loaded).